-
Publish Your Research/Review Articles in our High Quality Journal for just USD $99*+Taxes( *T&C Apply)
Offer Ends On
Julieth Kalikwendwa Kabagire* and Khadija Ahmed Shebe
Corresponding Author: Julieth Kalikwendwa Kabagire, Dermatology Unit, Internal Medicine, Kilwa Road Police Regional Referral Hospital P.O. Box 9791, Dar-es-salaam, Tanzania.
Received: March 19, 2025 ; Revised: April 10, 2025 ; Accepted: April 13, 2025 ; Available Online: April 17, 2025
Citation: Kabagire JK & Shebe KA. (2025) Sporadic Keratosis Follicularis (Darier’s Disease) in a Pediatric Patient: A Case Report. J Derm Allerg Res, 2(1): 1-3.
Copyrights: ©2025 Kabagire JK & Shebe KA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Views & Citations
Likes & Shares
Background: Keratosis follicularis, also known as Darier’s disease, is a rare autosomal dominant genodermatosis characterized by hyperkeratotic papules, particularly in seborrheic areas. This condition is caused by mutations in the ATP2A2 gene, which encodes a calcium ATPase pump crucial for keratinocyte adhesion. Although familial inheritance is common, sporadic cases account for approximately 40-50% of reported instances.
Case Presentation: We present the case of a 4-year-old boy with a two-month history of a pruritic rash that initially appeared on the scalp and progressed to the face, trunk, and extremities. The child had relocated to a humid, high-temperature environment shortly before symptom onset and had no family history of similar dermatologic conditions. Clinical examination revealed febrile illness, malodorous greasy hyperkeratotic plaques with brownish hyperpigmentation, and red streaks on several fingernails. Histopathological examination confirmed the diagnosis of Darier’s disease, showing epidermal hyperkeratosis with suprabasal clefting. The patient was treated with oral antibiotics, antifungal shampoo, topical retinoids, topical corticosteroids, and potassium permanganate baths, resulting in significant clinical improvement.
Conclusion: This case highlights a sporadic presentation of Darier’s disease in a pediatric patient, underscoring the importance of clinical recognition and histopathologic confirmation for timely intervention. Despite its rarity, the psychosocial impact and recurrent nature of the disease necessitate long-term management strategies.
Keywords: Darier’s disease, keratosis follicularis, ATP2A2 mutation, Pediatric dermatology, Sporadic case, Genodermatosis
INTRODUCTION
Darier’s disease, or keratosis follicularis, is a rare autosomal dominant genodermatosis first described by Ferdinand-Jean Darier in 1889. It results from mutations in the ATP2A2 gene on chromosome 12q23-24.1, which encodes the sarco/endoplasmic reticulum calcium ATPase (SERCA2) pump, essential for calcium homeostasis in keratinocytes. Disruption in calcium signaling due to ATP2A2 mutations leads to acantholysis and dyskeratosis, resulting in characteristic hyperkeratotic papules primarily in seborrheic areas, such as the scalp, face, chest, and back [1]. While the disease typically manifests in adolescence, earlier presentations in pediatric cases are observed.
Although Darier’s disease usually follows an autosomal dominant inheritance pattern, 40-50% of cases are sporadic due to de novo mutations [2]. The condition shows variable expressivity; some patients have mild, localized lesions while others develop severe disease. Environmental factors like heat, humidity, mechanical trauma, and infections can exacerbate symptoms [3]. Additionally, nail abnormalities, including red and white longitudinal streaks, and mucosal involvement, such as whitish papules on the oral mucosa, are common [4].
Histologically, Darier’s disease is characterized by acantholysis, dyskeratosis, and suprabasal clefting, differentiating it from other acantholytic dermatoses like Hailey-Hailey disease and pemphigus vulgaris. Immunofluorescence studies help distinguish it from autoimmune blistering diseases, as IgG and C3 deposition are absent at the epidermal level [5]. Treatment focuses on symptom management with topical retinoids, corticosteroids, and keratolytics to reduce hyperkeratosis, while systemic retinoids like acitretin are reserved for severe cases. The psychosocial impact of visible skin lesions in pediatric patients necessitates early diagnosis and long-term management strategies.
CASE REPORT
A four-year-old boy presented with a two-month history of an intensely pruritic rash that initially appeared on the scalp and progressively spread to the face, trunk, and extremities. The child had recently relocated from a cooler region to a humid, high-temperature environment. There was no family history of similar dermatologic conditions, and he had not used any medications prior to presentation.
Upon examination, the patient was febrile and appeared ill. His skin lesions consisted of malodorous, greasy, brownish hyperpigmented plaques affecting the scalp, face, trunk, and extremities, along with red streaks observed on several fingernails (Figure 1A).

LABORATORY AND HISTOPATHOLOGICAL FINDINGS
A full blood count revealed lymphocytosis. Histopathological examination demonstrated epidermal hyperkeratosis with suprabasal clefting, while the dermis exhibited mild focal infiltration by chronic inflammatory cells, predominantly macrophages and lymphocytes.
MANAGEMENT AND OUTCOME
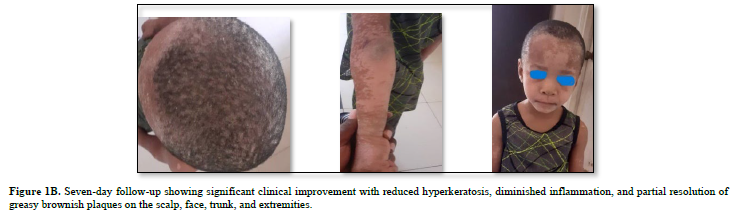
The patient was started on a combination of systemic and topical therapies to control symptoms, prevent secondary infections, and promote keratinocyte differentiation. He received oral antibiotics (amoxicillin/clavulanic acid, 375 mg PO BID for 7 days) to prevent secondary bacterial infections and ketoconazole shampoo to reduce yeast colonization and inflammation. Topical therapy included retinoids applied on alternate days to promote keratinocyte differentiation and topical corticosteroids (Betamethasone valerate 0.1%) to reduce inflammation. Additionally, potassium permanganate solution (1:1000) was used as bath water to assist with lesion debridement and infection control. At the 7-day follow-up, significant clinical improvement was observed, with reduced hyperkeratosis and inflammation (Figure 1B). Long-term follow-up was recommended to monitor for potential relapses and adjust treatment as necessary.
 DISCUSSION
DISCUSSION
Darier's disease, or keratosis follicularis, represents a complex interplay between genetic mutations and environmental factors leading to distinctive cutaneous manifestations. The ATP2A2 gene mutations responsible for this condition disrupt calcium homeostasis in keratinocytes, resulting in acantholysis and dyskeratosis [1,6]. This case report illustrates the sporadic occurrence of Darier's disease in a pediatric patient, emphasizing its unique presentation in a young demographic without a family history of similar dermatological conditions.
The patient's clinical presentation, characterized by pruritic, hyperkeratotic plaques in seborrheic areas, aligns with established descriptions of the disease [3,7]. The rapid progression of the rash and environmental changes likely contributed to symptom exacerbation, as environmental factors are known to influence severity [8]. The presence of malodorous plaques and nail abnormalities supports the diagnosis, as these features are commonly associated with Darier's disease [9].
Histopathological findings-epidermal hyperkeratosis with suprabasal clefting-are characteristic of Darier's disease, distinguishing it from other acantholytic dermatoses [10]. The absence of IgG and C3 deposition in immunofluorescence studies further confirms the diagnosis, highlighting the need for comprehensive histological evaluation in suspected cases.
The treatment regimen employed in this case, including oral antibiotics, antifungal shampoo, topical retinoids, and corticosteroids, is consistent with current therapeutic approaches. The combination of systemic and topical therapies proved effective, as evidenced by significant clinical improvement within a week. This rapid response underscores the importance of an individualized treatment strategy tailored to the patient's specific needs and disease severity.
The psychosocial impact of Darier's disease in pediatric patients is significant. Visible skin lesions can affect a child's quality of life, leading to social stigma and emotional distress [11]. Early recognition and appropriate management are essential not only for clinical outcomes but also for addressing the psychological well-being of affected children. Long-term follow-up is crucial to monitor for relapses and adjust treatment as necessary, ensuring comprehensive care for this chronic condition.
CONCLUSION
This case illustrates the sporadic nature of Darier's disease in a pediatric patient, emphasizing the importance of clinical awareness, histopathological confirmation, and a holistic approach to management. Given the rarity of this condition, ongoing education and research are vital to enhance understanding and improve treatment outcomes for affected individuals. Future studies should focus on identifying environmental triggers and refining therapeutic strategies to mitigate the impact of this challenging genodermatosis.
No Files Found
Share Your Publication :