-
Publish Your Research/Review Articles in our High Quality Journal for just USD $99*+Taxes( *T&C Apply)
Offer Ends On
Pallavi Kaulwar*
Corresponding Author: Pallavi Kaulwar, Ajeenkya DY Patil University, Pune, India.
Received: April 5, 2021 ; Revised: May 7, 2021 ; Accepted: May 10, 2021 ; Available Online: May 26, 2021
Citation: Kaulwar P. (2021) “The Clock is Ticking,”: Tuberculosis in United Kingdom. J Gene Cell Mol Biol, 1(1): 1-5.
Copyrights: ©2021 Kaulwar P. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Views & Citations
Likes & Shares
Abstract
Tuberculosis (TB) is a bacterial infection caused by the Mycobacterium tuberculosis (M.tb) bacteria that primarily affects the lungs. In the United Kingdom, tuberculosis is still a major public health issue. Given the disease's low overall incidence of 14 per 100,000, it is more common in major cities, among people born abroad, and other groups with unique risk factors. In the United Kingdom, migrant and racial minorities have higher tuberculosis (TB) rates than the general population. Historically, differential pathogen exposure due to migration from high-incidence regions and transnational relations maintained with TB endemic countries of birth or ethnic origin has been blamed for much of the difference in incidence between UK-born and migrant populations.
Tuberculosis is on the rise in the United Kingdom for a number of reasons. In the United Kingdom, there is no single intervention that can put tuberculosis under control; instead, a variety of interventions concentrating on different aspects of control is required. As a result, there is a widespread belief that migrants have a higher tuberculosis disease prevalence than the general population. Tuberculosis continues to be a significant cause of morbidity and mortality around the world. According to recent reports, its prevalence among the elderly is growing even in the developing world. Active tuberculosis symptoms are non-specific and less severe in the elderly. In the elderly, radiological characteristics are more likely to be "atypical," and skin tests are more often negative.
However, since it is essentially a disease of poverty, prevention goes beyond this. As a result, good ventilation and better living standards are welcomed, while overcrowding should be avoided. Another significant part of prevention is improving nutritional status.
INTRODUCTION
Tuberculosis (TB) is a bacterial infection caused by the bacteria Mycobacterium tuberculosis (M.tb) that most often affects the lungs. Inhalation of infectious particles released by close contacts is how M.tb infection is acquired [1]. Despite the fact that low- and middle-income countries account for over 90% of tuberculosis (TB) cases, a global outbreak of TB has affected high-income countries such as the United Kingdom. The incidence of tuberculosis in the United Kingdom follows a similar trend to that of other European countries, rising by 25% in the last decade. There are significant variations in the prevalence of tuberculosis among the different ethnic groups.
Tuberculosis remains a significant public health concern in the United Kingdom. Despite the low overall incidence of 14 per 100 000, the disease is more prevalent in major cities, among people born overseas, and other groups with particular risk factors. In the United Kingdom, the United States, and many eastern and western European countries, prisoners are known to be at a higher risk of tuberculosis. In the United Kingdom, citizens born outside the country account for the majority of tuberculosis cases (73 percent in 2009). After several years, the majority develop active symptomatic disease (in 2009, almost four fifths had lived in the UK for two or more years). The majority of cases, according to DNA fingerprinting tests, resulted from latent Mycobacterium tuberculosis infection acquired outside the UK.
M tuberculosis is transmitted through aerosol transmission and disproportionately affects marginalized urban communities that cluster geographically (for example, homeless people, drug users, and offenders), arrive late to medical care, follow prescription regimens poorly, and have low treatment completion rates. Sputum smear positive pulmonary disease makes them more infectious than other tuberculosis patients, and they have a high rate of drug resistance. As a result, social isolation has an effect on existing tuberculosis rates [2]. People with latent M tuberculosis infection are more likely to develop active tuberculosis whether they have HIV, diabetes, chronic kidney disease, or are taking anti-tumor necrosis factor medications. HIV infection is more common in the areas of the world where most non-UK born tuberculosis occurs, and HIV coinfection accounts for 2-10% of tuberculosis cases in the UK.
Tuberculosis rates in the UK have now surpassed those of all other Western countries, with the exception of Spain and Portugal, where rates are declining in comparison to the UK. The main distinction is that migrants come from different parts of the world. The Indian subcontinent and Sub-Saharan Africa have a higher proportion of UK migrants from countries with a high prevalence of tuberculosis. Foreign-born people of the United States also have higher tuberculosis rates. However, tuberculosis rates in both foreign and US-born residents have decreased, while rates in native-born people in the UK have remained constant while rates in non-UK-born people have increased.
EPIDEMIOLOGY
Immigrant populations and tuberculosis
Because of the high prevalence of tuberculosis among migrants from high-burden countries, NICE recently lowered the screening threshold for latent M tuberculosis infection to immigrants from countries with a 40/100 000 active tuberculosis rate. 16 According to a recent economic study, a threshold of 150/100,000 could be more acceptable. The use of a higher threshold would allow resources to be directed to previously underserved areas. The need for improved information collection and sharing systems that connect arrival data with local NHS and social services is highlighted by the inadequate local follow-up of people at high risk. This will allow local services to provide newcomers in their area with primary care registration and a health check (NHS England). In Hackney, London, a cluster randomized controlled trial of an educational programme supporting tuberculosis assessment in people registering in primary care26 enhanced active tuberculosis detection 1.68-fold (95 percent confidence interval 1.05 to 2.68) and latent infection threefold (0.98 to 9.20); BCG coverage increased 9.52-fold (4.0 to 22.7). This highlights the importance of locally tailored solutions.
Hard to reach groups
The English Department of Health agreed to finance a pilot "Search and Treat" programme in response to the high rate of follow-up failure among hard-to-reach communities. People with suspected tuberculosis who were diagnosed by mobile chest radiography units were provided assistance in navigating the health and social care system, which was also achieved with the aid of non-profit organizations. Assuring safe and secure housing is an easy measure (Department of Health and Social Care UK). It's also possible to boost detection in jails. While several prisons are about to begin chest x-ray screening, most tuberculosis assessments are done on an ad hoc basis based on symptoms [2].
Healthcare administration
Neither the NICE guidelines nor the national commissioning toolkit has an effective care model. The NHS's proposed changes provide a chance to boost public health, but they must not impede the need for a coordinated service. Devolving commissioning to local providers could harm tuberculosis control. Tuberculosis outbreaks, for example, are unlikely to occur frequently within each clinical commissioning group's region or to cross many financial and administrative boundaries. As a result, it's unlikely that any single commissioning committee has budgeted for the resources needed to deal with an outbreak at a school. Similarly, treating multidrug-resistant and extensively drug-resistant tuberculosis is costly, and management will be best financed by a broader grouping. This can necessitate sub-national commissioning through the NHS Commissioning Board and close ties with Public Health England (NHS, England).
Susceptibility of children to develop tuberculosis. Common and severe forms of disease
Estimating the global burden of tuberculosis in children is difficult, owing to the difficulty in identifying and verifying the disease. Furthermore, the lack of a common case description and the prevalence of extra pulmonary disease make reliable data on pediatric tuberculosis difficult to obtain. Children are more likely to become infected and develop disease after being exposed to a sputum smear-positive source case in the home. Even household contacts with smear-negative tuberculosis can infect children. Infection in children under the age of five suggests a possible source case in the home. As a consequence, TB in children under the age of five shows recent and/or continuing transmission.
The most common types of pediatric tuberculosis are pulmonary disease and intrathoracic adenopathy, which account for 60-80 percent of all cases. 25 Infants and young children are more likely than older children to develop serious types of pediatric tuberculosis (disseminated TB and TB meningitis). Perinatal tuberculosis (congenital and neonatal) is a life-threatening disease with a 50% mortality rate. Congenital tuberculosis is unusual and is related to tuberculous endometritis or disseminated tuberculosis in the mother. Neonatal tuberculosis is caused by an infant’s exposure to the mother’s respiratory secretions and is much more common.
Patients and healthcare staff from Somalia in the United Kingdom
Despite the fact that over 90% of tuberculosis (TB) cases occur in low- and middle-income countries, the disease has resurfaced in high-income countries, including the United Kingdom. The incidence of tuberculosis in the United Kingdom follows a similar trend to that of other European countries, with a 25% rise over the last decade. There are significant variations in the incidence of tuberculosis among the UK population, with 73 percent of cases occurring in people born outside the UK, with Somalis constituting the third largest group. Nurses play an important part in the prevention and treatment of tuberculosis. Nurses must recognize that tuberculosis is a disease with sociocultural as well as physical consequences [3] and they must consider how people of various ethnic backgrounds view the disease. The current research looks at how people of Somali descent in the UK deal with tuberculosis from the start of symptoms to the end of treatment. Such information is useful in assisting nurses in reducing the global effect of tuberculosis. Diagnostic delays caused by patients' unwillingness to seek medical advice are most common in societies where tuberculosis is highly stigmatized, resulting in social isolation of TB patients. When friends withdrew from social experiences, a minority of patients experienced isolation. The social stigma faced by these patients was attributed to a lack of understanding of tuberculosis in the Somali community, especially a false belief that it could be transmitted by sharing eating utensils [3].
TB VACCINE DEVELOPMENT
Van Der Meeren and colleagues published the interim results of a phase 2b efficacy trial of a protein and adjuvant candidate tuberculosis vaccine, M72 and AS01e, in HIV-uninfected adults with M tuberculosis latent infection in Africa in 2018, after a mean follow-up of 23 years. In this interim study, the M72 plus AS01e group showed a 540% (95 percent CI 29%-782) reduction in bacteriologically confirmed active pulmonary tuberculosis disease relative to the placebo group (p=004). 23 Since it demonstrates proof of concept and biological viability in humans, this notable result has reignited interest in tuberculosis vaccine production. An age is noteworthy. This result may be explained by the fact that people who have been contaminated recently are easier to protect. Significant questions, however, remain unanswered. The long-term durability of this protective effect is unknown, so data from the final study will be crucial [4]. Evidence from preclinical animal models indicates that administering a vaccine directly to the respiratory mucosa, which mimics the natural route of infection, could be a more protective route of vaccination than intradermal or intramuscular administration [4].
TB IN ELDERLY
In the United Kingdom, mortality rates have dropped significantly in the last 50 years, as half of all smear-positive patients died within two years. The increase in general health and social conditions, as well as the growth of effective therapy, has led to the decrease in mortality [5]. While research in the United States have indicated that elderly patients in residential homes are at a higher risk of tuberculosis, this has not been repeated in the United Kingdom. In the UK, tuberculosis is still prevalent among ethnic minority groups: 121 per 100,000 in subjects from the Indian subcontinent, 210 per 100,000 in Black Africans, and 26 per 100,000 in Black Caribbeans, compared to 4.4 per 100,000 in the general population. As a result, even in developed countries, tuberculosis remains a major public health concern, and physicians must maintain a high index of suspicion, especially in the elderly [5].
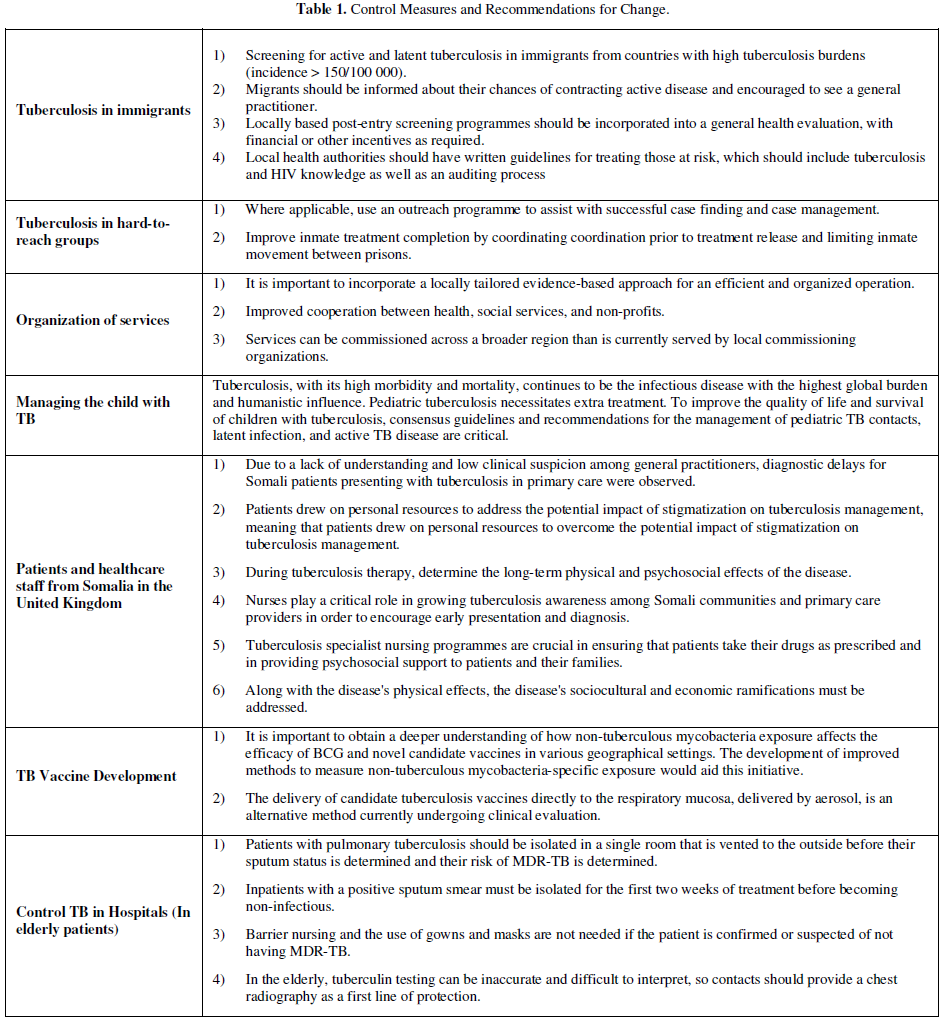
Control Measures and Recommendations for Change (Table 1)
DISCUSSION AND CONCLUSION
The growth of tuberculosis in the United Kingdom is attributed to a variety of reasons. There is no single intervention that can bring tuberculosis under control in the United Kingdom; instead, a number of interventions focusing on various aspects of control are required. We are pleased that one of the steps in the government's Public Health Results Framework is the completion of tuberculosis care (PHE, England).
This study's results shed light on the perspectives of Somali TB patients in the United Kingdom, from the onset of symptoms to diagnosis, care, and coping with the disease. The majority of research on TB patients' experiences has taken place in low-income countries, where the disease is more common, or on recent migrants to high-income countries [3].
In the last two decades, significant progress has been made in the manufacture of tuberculosis vaccines. In two efficacy trials, a biological signal of efficacy was discovered. Preclinical animal models are being used to test promising candidate vaccines at an earlier stage of production. Furthermore, progress has been made in the understanding and recognition of the defensive immune response. New tools like practical in-vitro assays and CHIMs could make vaccine production and selection even easier. Many questions, however, remain unanswered. Parallel to preclinical animal studies and further fundamental science to identify protective immune mechanisms, it is critical to advance promising candidate vaccines into well-designed human efficacy trials.
Even in developing countries, tuberculosis is a leading cause of morbidity and mortality. Symptoms may be ambiguous, and clinical and radiological observations in the elderly do not necessarily correlate to those seen in post-primary tuberculosis. Since diagnoses are often missed or delayed, it is important for physicians caring for the elderly patient to be diligent.
Tuberculosis, with its high morbidity and mortality, continues to be the infectious disease with the highest global burden and humanistic influence. Pediatric tuberculosis necessitates extra care. To improve the quality of life and survival of children with tuberculosis, consensus guidelines and recommendations for the management of pediatric TB contacts, latent infection, and active TB disease are critical.
Most significantly, government commitments are strongly promoted so that the World Health Organization and all other foreign organizations engaged in tuberculosis control can effectively eliminate the disease from all populations.
Hence, it is a common misconception that migrants have a higher prevalence of tuberculosis disease than the general population in the United Kingdom. In order to enact successful strategies to combat tuberculosis in these vulnerable communities, it is critical to consider the nuanced and multifactorial drivers of this discrepancy.
So, in future, this momentum must be maintained in order to inspire the next generation of clinicians and scientists to pursue careers in this area. If we are to build on recent progress and eventually produce, license, and deploy a widely effective tuberculosis vaccine, we will need long-term, collaborative funding and working models, as well as open data sharing. Only then will we be able to fulfil the long-awaited task of eradication.
REFERENCES
No Files Found
Share Your Publication :