-
Publish Your Research/Review Articles in our High Quality Journal for just USD $99*+Taxes( *T&C Apply)
Offer Ends On
Konstantina Metaxouli*, Chrysoula Tsiou, Eleni Dokoutsidou and Nikoletta Margari
Corresponding Author: Metaxouli Konstantina, PhD(c), Department of Nursing, University of West Attica, Egaleo, Athens, Greece.
Received: December 11, 2023 ; Revised: January 05, 2024 ; Accepted: January 08, 2024 ; Available Online: January 18, 2024
Citation: Metaxouli K, Tsiou C, Dokoutsidou E & Margari N. (2024) Functional Disability, Its Relationship to Eating Habits, Sociodemographic Characteristics, and Clinical Features of Patients with Multiple Sclerosis. J Nurs Midwifery Res, 3(1): 1-8.
Copyrights: ©2024 Metaxouli K, Tsiou C, Dokoutsidou E & Margari N. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Views & Citations
Likes & Shares
Introduction: The relation between functional capacity and dietary habits of individuals affected by Multiple Sclerosis (MS) has attracted considerable interest worldwide. However, relevant data for Greece are scarce.
Aim: Investigate the relation between the physical health of individuals with MS and their dietary patterns, as well as their socio-demographic and clinical characteristics.
Materials and Methods: 137 patients with relapsing-remitting MS who visited the Neurological Department, of a Public Hospital in Nice Attica Greece, were included. Patients’ demographic characteristics were recorded. Functional disability was assessed with the Revised Multiple Sclerosis Rating Scale (MSRS-R), which is not widely used. Dietary habits were assessed with the following dietary intake frequency scales - The Mediterranean Diet Score (Med Diet score) and nutrition assessment - Mini Nutritional Assessment (MNA).
Results: The response rate was 100% (137 patients responded). The Med Diet score was not significantly related to the MSRS-R score, unlike the overall MNA score, which presented a significant negative relation with MSRS-R score. 75.2% of the participants were women. Greater functional impairment was found in older patients (p<0.001). Additionally, patients who had completed primary/secondary/high school education (p=0.026), those who were employed (p=0.011) and smokers (p=0.044) reported greater functional difficulty. Greater functional impairment was significantly associated with lower economic status (p=0.044).
Conclusions: The results suggest that increasing age, lower socioeconomic status, smoking and poor dietary habits are related to decreased functional capability in patients with MS. The findings of the present study need to be replicated in larger, controlled trials.
Keywords: Multiple sclerosis (MS), Functional disability, Nutrition, Clinical features, Demographic characteristics
Abbreviations: MS: Multiple Sclerosis; MSRS-R: Multiple Sclerosis Rating Scale-Revised; Med Diet Score: The Mediterranean Diet Score; MNA: Mini Nutritional Assessment; ΒΜΙ: Body Mass Index; RRMS: Relapsing-Remitting MS; PPMS: Primary Progressive MS; SPMS: Secondary Progressive MS
RESEARCH HYPOTHESIS
Increasing age, smoking, employment status, lower socioeconomic status and up to secondary education level were statistically related to higher functional incapacity.
The MNA score was significantly related to the MSRS-R score.
Contrariwise, the Med Diet score did not present any relation with the MSRS-R score.
Higher functional disability (MSRS-R) was inversely related to good nutrition as signified by the MNA score.
BACKGROUND
Multiple sclerosis (MS) is a chronic inflammatory neurological disease of considerable diversity. Clinical manifestations of the disease include abnormal walking patterns, limb weakness, loss of consciousness, muscle pain, fatigue, cramps, optic neuritis, speech impairment, cognitive dysfunction, anxiety, depression, gastrointestinal disorders, urinary incontinence, and sexual dysfunction [1-3]. The disease presents in three forms, a) relapsing-remitting multiple sclerosis (RRMS), which is the most common, b) primary progressive multiple sclerosis (PPMS), and c) secondary progressive multiple sclerosis (SPMS). Currently there is no cure for MS, whilst the disease’s course remains unclear [4]. Genetic and environmental factors have been implicated in the etiology of the disease. The most important environmental risk factors include exposure to Epstein Bar virus (EBV), smoking, limited sun exposure, vitamin D3 deficiency, vitamin B12 deficiency, alcohol consumption and obesity [5,6]. The course of MS appears to be affected by diet, as obese individuals seem to face a higher risk of developing MS when compared to normal weight individuals, with the relevant rate increasing with prior EBV infection [7,8]. Individuals who adhere to a specific nutrition plan present improved physical health [9,10]. Whereas physical activity, mental exercise and social participation also have a positive effect, in the sense that they decrease the severity of symptoms [10]. Physical activity may also reduce the number of recurrences of the disease [11]. In general, behaviors that promote a healthy lifestyle such as a balanced diet and exercise have been reported to improve well-being of individuals with MS [9,12]. Maintaining a good functional status, in tandem with proper management of symptoms, is crucial for people with MS. Functional capacity is a significant cause for concern not only among sufferers in Greece, but is also of global interest, since the fear of impending disability is common to all patients and their families. To date, relevant studies have not been conducted in Greece, unlike other European countries. In the present study, the application of the MSRS-R scale, the revised multiple sclerosis assessment scale, whose use has been relatively limited, even among international researchers, was selected. The MSRS-R is the shortest, simplest and easiest self-administered scale for people with MS. It focuses on eight functional areas, with minimal word length [13]. The belief that a healthy lifestyle and diet may help MS patients delay the progression of their disease may encourage them to adopt it. Therefore, the establishment of a relationship between disease progression and several socio-demographic and medical characteristics, such as age, gender, employment, education, socioeconomic status, smoking, can broaden significantly our knowledge about whether patients are able to adhere to better eating habits and a healthier lifestyle.
METHODS
Study Design
This cross-sectional study was carried out in a public hospital, in the region of Attica (General Hospital of Nice). The sample consisted of one hundred and thirty-seven (137) adults, diagnosed with relapsing-remitting MS, who presented to the hospital’s Neurological Department for follow-ups or treatment. The present study attempted to identify relations between the functional disability of MS patients, using the scale (MSRS-R), and there: a) socio-demographic characteristics, b) medical history and c) dietary habits. For the latter, the dietary intake frequency scales - The Mediterranean Diet Score and nutrition assessment - Mini Nutritional Assessment MNA were utilized [14,15]. Inclusion criteria were a) patients with relapsing-remitting MS presenting at the outpatient clinics, with odd registration number, b) individuals ≥ 18 years old, c) diagnosis of the disease at least 6 months prior, d) good understanding of the Greek language, and e) willingness to participate in the study. Exclusion criteria were a) cortisone administration, modification of treatment, participation in a clinical trial, within the last 6 months and b) patients with psychiatric disorder. The data collection instrument was a questionnaire administered by the researcher, in the context of a fifteen-minute personal interview with patients. Data were collected at the hospital premises during the period from June 2021 to May 2022. After being informed and consenting to participate in the study, participants provided information regarding their demographic-social characteristics and medical history, as well as responded to the questions comprising the MSRS-R, Med Diet score, and MNA questionnaires. The participation rate was 100%. For this study approval was given a) by the Ethics and Deontology Committee (E.H.D.E) of the University of Western Attica (P.D.A.) (19th/ 07-06-2021) and b) by the Scientific Committee of the General Hospital of Nicaea Piraeus (issue ID.16th, decision of the 21st /02-09-2020). These measures ensure that the study was conducted in accordance with ethical standards as defined in the 1964 Declaration of Helsinki and its subsequent amendments or comparable ethical standards. All participants provided written informed consent.
QUESTIONNAIRES
The MSRS-R scale is a useful tool for both sufferers and health professionals [16,17]. Is a concise measure of MS-related functional disability. MSRS-R correlated well with comparison instruments, such as MSIS-29, MSWS-12, and PRIMUS. The MSRS-R exhibited high internal consistency (Cronbach's alpha =0.86) and 1-week retest reliability (r = 0.91). Consisting of 8 items, it measures the impact of MS on patients and more specifically in terms of the course of the disease, treatment effects, side effects and relapses. The MSRS-R is released for use under Creative Commons license [13]. The Med Diet questionnaire is a popular questionnaire measuring adherence to the Mediterranean diet [18,19]. It was developed by Greek professors and applied to the participants (3.042) of the ATTICA study in the Greek population. The Med Diet questionnaire examines a variety of foods with complex combinations of nutrients. The diet score assesses adherence to the Mediterranean diet. This score is a useful tool for the assessment of an individual's nutritional status and for clinical and research purposes. The Med Diet Score has been found valid and repeatable in previous works. The questions cover 156 foods and beverages that belong to the following 11 food groups: refined grains, fruits, vegetables, legumes, potatoes, fish, meat, poultry, full-fat dairy products, olive oil and alcohol. The total score ranges from 0 to 55, indicating that the higher the score, the greater the adherence to the Mediterranean diet [14]. The Mini Nutritional Assessment is a validated nutrition assessment tool consisting of 18 items. The MNA is accurate in identifying nutrition risk. The MNA is an assessment tool with a reliable scale usable by healthcare professionals and it should be included in the geriatric assessment [20,21]. The first 6 questions provide an assessment of nourishment level. The other 12 questions provide a general nutritional assessment. The sum of both scores presents the overall nutrition assessment indicating either normal levels of nutrition or risk of malnutrition or undernourishment [15].
Statistical Analysis
Quantitative variables were expressed as means (Standard Deviation) or as medians (interquartile range). Qualitative variables were expressed as absolute and relative frequencies. Mann-Whitney and Kruskal-Walli’s test were utilized for the comparison of mean values between groups. Spearman’s rho correlations coefficients were used to investigate the potential association between two continuous variables. Multiple linear regression analysis was utilized with dependent variable the MSRS-R scale in a stepwise method (p for entry 0.05, p for removal 0.10). The regression equation included terms for all patients’ demographics, information for their disease, as well as their dietary habits. Adjusted regression coefficients (β) with standard errors (SE) were computed on the basis of the results derived from the linear regression analyses. The logarithmic transformation of MSRS-R scale was used in the regression due to lack of normality. All reported p values are two-tailed. Statistical significance was set at p
RESULTS
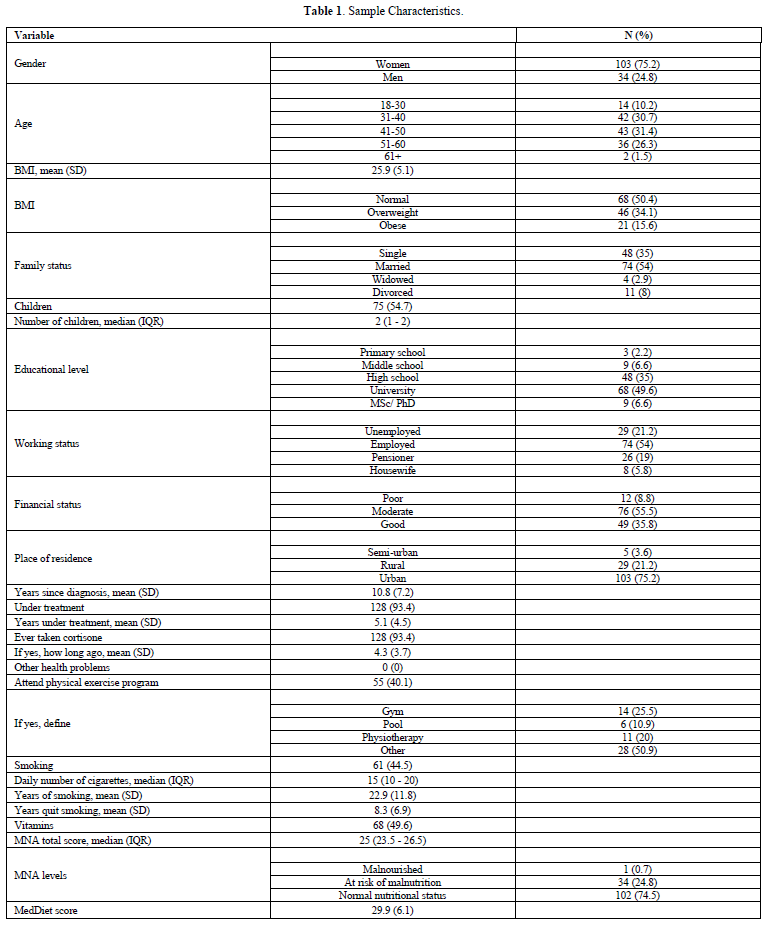
The sample consisted of 137 patients with MS. The majority of the patients were women (75.2%), 41-50 years old (31.4%) and with normal BMI (50.4%) Their characteristics are presented in Table 1. Almost half of the patients (49.6%) were university graduates, 54.0% were employed and 55.5% were of moderate financial status. Additionally, mean time since diagnosis was 10.8 years (SD=7.2 years). The majority of the patients had normal nutritional status (74.5%) and mean Med Diet score was 29.9 (SD=6.1).
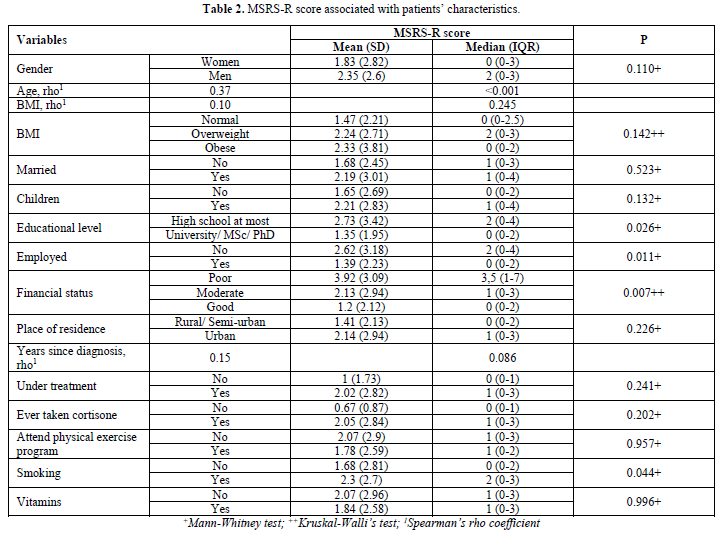
As presented in Table 2, older patients, high school graduates at most, employed and smokers faced greater functional difficulties. Additionally, greater functional difficulty was significantly associated with lower financial status.
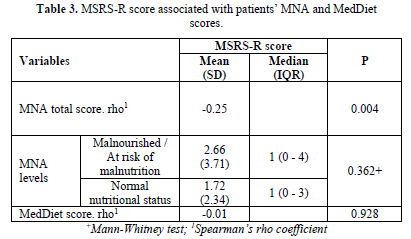
The Med Diet score was not significantly associated with the MSRS-R score Table 3. On the contrary, the MNA total score was significantly and negatively associated with MSRS-R score, indicating that normal dietary habits were associated with lower functional disability. However, there was not a statistically significant difference between the two distinct MNA levels.
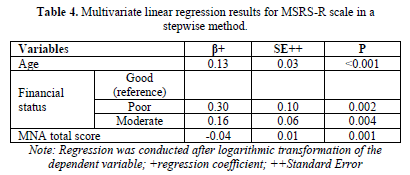
The multivariate linear regression analysis revealed that increasing age was associated with greater MSRS-R scores Table 4. Also, patients with lower or moderate financial status presented significantly greater functional disability when compared to patients with good financial status. Moreover, a greater MNA score, i.e., indicating more normal dietary habits, was significantly associated with a lower MSRS-R score.
DISCUSSION
The majority of patients were female, with a 1:3 male-to-female ratio, whilst belonging to the 41–50-year group. This finding is in line with other studies. In a cohort study with 952 participants from Australia, the male-female ratio was 1:4 with 82.9% of MS patients being women [9]. A similar ratio appears in sub-Saharan Africa (1:4 in favor of women) [22]. However, whether women are more susceptible to MS remains unknown. A study that used mice in order to investigate the effect of gender on neurodegeneration and autoimmunity concluded that T lymphocytes play a role, yet that finding is questionable [23]. Women during their lifetime are subjected to strong hormonal modifications. A study identified female hormones, specifically estrogen, progesterone, and testosterone, as being implicated in MS in women. In the post-menopausal period, less inflammatory activity appears to occur in the context of MS disease [24]. The existing evidence suggests that women are diagnosed earlier and present more relapses, whilst developing a greater number of atrophies and lesions. Nevertheless, they appear to suffer from a milder form of the disease comparing to men. The underlying causes of this once again remain unknown. It has been hypothesized that the female peripheral immune system responds more effectively by limiting MS activity [25,26]. MS is considered to be the first cause of physical disability in young and middle-aged patients [10]. In our study, approximately half of the patients were employed, while the remaining were unemployed or retired (21.2% and 19%, respectively, p=0.11). According to the findings of a study, 50% of patients with MS will not be able to carry out their daily tasks within ten years of developing the disease [27]. At their most productive age, they are faced with a serious illness, whilst simultaneously having to deal with financial and work-related issues and potentially unemployment. The symptoms of the disease often affect the patient’s daily activities, such as their vocational rehabilitation, resulting in their losing or struggling to find work, resulting thus in a considerable financial burden [28]. A study by Vozikis and Sotiropoulos [29], published in Greece in 2012, highlighted the lack of data with regard to the economics of the disease. The cost of MS, which is very high internationally, increases with the severity of the disease, and many patients do not work. This implies that the average annual total cost born by MS patients in Greece, accounting to 8,334 euros, is practically unbearable for an unemployed patient [29].
Accordingly, the difficulties arising from the patients' unemployment status decisively affect their lives and health. A recent study showed that economic status was inversely related to future disability in MS [30]. In the same vein, another study showed that a lower socioeconomic status increased the risk of disability [31]. Additionally, much needed treatments may not be carried out due to unavailable financial resources. In recent years, health promotion programs for people with disabilities have been developed [32]. The implementation of such programs, e.g., publicly funded programs providing favorable working conditions and hours to support MS patients, who wish to work, could be a solution. The majority of patients included in our study reported a satisfactory financial status. A low percentage, 8.8% reported poor, while 55.5% and 35.8% reported a moderate and good financial status, respectively. It should be noted that the financial burden that medication, examinations, and hospitalizations of MS patients place on healthcare systems is particularly high [27]. These costs are exacerbated if patients need treatment in specialized centers to restore their functional capacity, whilst limited access to these facilities also present an important issue. It is not uncommon for MS patients to pay for several additional treatments out of their pockets [33]. In our study older people showed higher rates of disability (p<0.001), a finding that is expected, as older people experience disabilities whether they have MS or not, due to aging. These disabilities may include memory disorders, arthritis, diabetes, cardiovascular disease, metabolic disorders etc. Age, as shown in a cohort study with 26,058 participants, is a factor contributing to increasing disability in MS [34]. A recent report points out that MS patients face an additional physical health burden of about 15-30 years when compared to their healthy peers [35]. Almost half of the participants in our study were university graduates and 6.6% were masters or doctorate holders. It has been posited that a higher educational level is related to the adoption of a healthy lifestyle in MS patients, which in turn can affect the disease and its progression [32]. Adopting a healthy lifestyle can have a significant impact on reducing the consequences of MS and may enhance physical and mental capacity, elements of paramount importance for patients' lives. It seems that a higher educational level positively affects information seeking behaviors, increased awareness about the disease, as well as skills acquisition, so as to better deal with it. Considering that smoking is a well-known risk factor of the disease, one might have expected lower rates of smoking among the study participants. Almost half of the participants (44.5%, p=0.44) reported a history of tobacco smoking. It seems that cigarette smoke creates an inflammatory environment that affects T lymphocytes and the function of the blood-brain barrier (BBB). Even passive smokers seem to be adversely affected, depending on their exposure to smoke, while occasional smokers also face an increased risk of developing MS [36]. Female smokers seem to face greater risk of developing MS compared to male smokers, but the underlying mechanism is yet to be elucidated [37]. Regarding nutrition in our study, a relation was found between the functional disability scale (MSRS-R) and the total score of the nutrition scale (MNA), in contrast to the Med Diet scale where no relation was found. Accordingly, a search conducted on databases PubMed, Medline, Scopus, and Google Scholar found no study within the last ten years that provided a relation between the scales MSRS-R and Med Diet. Normal eating habits are associated with decreased functional disability, as they provide the body with the necessary vitamins, minerals, and other nutrients to maintain physical health and mental function. A balanced diet, which is rich in vegetables, fruits, whole grains, lean proteins, and healthy fats, helps maintain energy levels, improve cognitive function and reduce inflammation. The consumption of adequate amounts of fiber reduces the risk of chronic diseases such as MS [38]. Healthy eating can help improve mood, reduce the risk of depression, and can better support overall physical health, leading thus to decreased functional disability [39,40]. A lifestyle involving lack of exercise, sedentary life, harmful eating habits and obesity, has led to an increase in the prevalence of MS. The majority of study participants (50.4%) presented a normal BMI, while overweight and underweight patients accounted for 34.1% and 15.6%, respectively. Obesity appears to be responsible for a mild but chronic inflammatory state and may therefore be associated with immune diseases. By affecting the cellular immune response to infections, obesity seems to increase the prevalence or worsen the prognosis of immunological diseases [41]. The findings of a study suggested that obesity was associated with increased rates of relapse, as well as the progression of the disease from a clinically isolated symptom to an established diagnosis of MS [42]. A high BMI in early life has been associated with a high risk of MS in adulthood. Adequate evidence supports the notion that a healthy lifestyle and diet seem to be related to decreased functional disability, while the symptoms of MS appear milder with fewer relapses [43,44]. Consistent with the results of previous studies, a survey of 1,490 MS patients in Australia suggested that a healthy lifestyle and a balanced diet improve physical and mental life [45]. The present study faces several limitations including the small sample size, as well as the fact it was conducted in a single healthcare institution. The specific public hospital was selected due to the existence of an organized Neurological Clinic, where a significant number of patients with MS are monitored. For practical reasons, this enabled the researchers to focus more adequately on the research goals. The coronavirus pandemic was a factor that deterred the collection of a larger sample, as several patients turned to paperless prescription and avoided hospital visits. Nevertheless, respondents were very positive about responding and participating in the study. The small sample size does not allow for the generalization of the results and findings of the study to the entire population of patients with MS in Greece. Therefore, the findings of the study are merely indicative. In addition, the self-rating of people with MS, on the MSRS-R scale, was subjective and thus systematic error may have been introduced.
CONCLUSION
In conclusion, it is believed that a healthy lifestyle and a good nutritional status play an important role in the management of symptoms and the progression of the disease. Preventive strategies can direct individuals to modify their lifestyles and adopt new management strategies. The exploration of the disease, which affects and therefore concerns thousands of patients, must continue in all directions, may it be genetic or environmental factors, since both contribute to the risk of the disease. Improved means of subsistence and satisfactory nutrition and exercise status are preventive practices that can contribute to improving the clinical course and quality of life of MS patients.
No Files Found
Share Your Publication :