-
Publish Your Research/Review Articles in our High Quality Journal for just USD $99*+Taxes( *T&C Apply)
Offer Ends On
Mutinke Zulu*, Kabwe Chitundu, Sebean Mayimbo, Samson Shumba, Nedah Chikonde Musonda, Deborah Nayame Mushamba, Patricia Katowa-Mukwato and Lonia Mwape
Corresponding Author: Mutinke Zulu, University of Zambia, School of Nursing Sciences Lusaka, Zambia.
Received: October 11, 2023 ; Revised: October 31, 2023 ; Accepted: November 03, 2023 ; Available Online: November 17, 2023
Citation: Zulu M, Chitundu K, Mayimbo S, Shumba S, Musonda NC, et al. (2023) Anxiety and Utilization of Counselling Services during COVID-19 Pandemic among Nurses and Midwives in Selected Urban Hospitals in Lusaka, Zambia. J Nurs Midwifery Res, 2(1): 1-9.
Copyrights: ©2023 Zulu M, Chitundu K, Mayimbo S, Shumba S, Musonda NC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Views & Citations
Likes & Shares
Introduction: Caring for patients with COVID-19 is physically and emotionally stressful. Inadequate Personal Protective Equipment increases fears and anxieties of contracting the infection. Provision of counselling services to nurses and midwives is one coping strategy. In this study, nurses and midwives at the Women and New-born Hospital and First Level Hospitals in Lusaka, Zambia, had their anxiety levels and use of counselling services evaluated.
Methodology: This was a cross-sectional study conducted between December 2020 and May 2021.The total sample was 167 participants, 79 nurses and 83 midwives. The setting was the Women and New-born Hospital and five first level hospitals in Lusaka, Zambia. The health facilities and participants were selected purposefully. Ethical considerations were observed. Data were collected using self-administered semi structured questionnaire and Hospital Anxiety and Depression Scale with a 14-item, self-report questionnaire. Data were analyzed electronically and associations between variables were measured statistically.
Results and Discussion of findings: Majority, 25 (86.21%) of female respondents had presence of anxiety compared to males 4 (13.79%). A survey conducted in Ethiopia reported that females’ nurses were more predisposed to anxiety and mood disorders. This could be due to various factors such as genetic, biological, hormonal, social, psychological factors including role pressure, difficulty in balancing work life, and inadequate support. This study showed that qualification and the research setting were significantly associated with anxiety with a P value of 0.017 and 0.013 respectively. Presence of anxiety was high in Kanyama (33.33%) and Chawama (33.33%). These first level hospitals are government owned and are highly populated; most often lack Personal Protective Equipment and face shortage of nurses and midwives, which worsens the anxieties among nurses and midwives. A similar study in Ethiopia reported that midwives who worked in government hospitals were more likely to experience anxiety compared to those that worked in the private hospitals. Only 42.51% (71/167) were aware about the availability of counselling centers, and most 68.57% (24/35) of them were working in antenatal clinics. Lack of awareness of counselling services among would affect utilization of counselling services.
Conclusion: The COVID-19 pandemic increased anxiety levels among nurses and midwives. Providing counselling services as well as Personal Protective Equipment can reduce the psychological stress related to stressful care giving.
Keywords: Anxiety, Counselling, COVID-19, Pandemic, Nurses, Midwives
INTRODUCTION
The novel COVID-19 emerged from Wuhan City in China and was reported to the World Health Organization (WHO on 31st December, 2019 [1]. Zambia, like any other country, was not spared from the COVID-19 pandemic. The first two cases of Coronavirus in Zambia were reported on the 18th of March, 2020 [2]. As of 16th August, 2020, Zambia had recorded a total of 9,186 laboratory confirmed cases of COVID-19 of which 56 were health including 21 nurses and midwives [3,4]. Nurses and Midwives risked contracting the infection as they were at the front line of care provision [5,6]. Caring for patients with infectious diseases such as COVID-19 is both physically and emotionally stressful. COVID-19 led to emotional distress and trauma [7]. Additionally, inadequate supply of Personal Protective Equipment put nurses and midwives at higher risk of contracting the infection which consequently increases their fears and anxieties of contracting the Virus and infecting their families. A study conducted in the Middle East on Coronavirus epidemic impact on health workers’ risk perceptions, work and personal lives reported that more than 80 percent of the health care staff expressed high anxiety levels of contracting the disease and transmitting it to their families [8,9]. Mental health care for health workers should be incorporated in the fight against COVID-19 [10]. Another study conducted in the Anhui Province of China to investigate emotional responses and coping strategies revealed nurses and nursing students showed higher levels of anxiety in females compared to the male nurses. In the same study, participants from the urban areas exhibited more anxiety compared to the ones from the rural areas [11]. They expressed fear and anxiety of contracting the Virus and infecting their families. Despite the magnitude of the problems being encountered, the nurses and midwives reported that no counselling services were being offered to them. Inadequate supply of PPE further puts nurses and midwives at higher risk of contracting the infection which consequently increases their fears and anxieties [12]. This study aimed at assessing the anxieties and utilization of counselling services among nurses and midwives attending to women at the Women and New Born Hospital and First Level Hospitals in Lusaka, Zambia.
MATERIALS AND METHODS
This was a cross-sectional study conducted between December 2020 and May 2021. The study was conducted at the Women and New-born Hospital and five first level hospitals in the Lusaka Urban District, namely Chilenje, Kanyama, Chipata, Matero, and Chawama. The health facilities and participants were selected purposefully because they provided primary health care services to clients including those with COVID- 19. Purposive sampling method was equally used to select 167 participants that included nurses (79) and midwives (83) who were involved in care provision for women who may have been asymptomatic or symptomatic and positive for COVID-19. Ethical approval was sought from the Biomedical Research Ethics Committee and the National Health Research Authority. Consent was obtained from the participants. Utilizing special codes to identify participants allowed for the preservation of anonymity and privacy. Participation was voluntary, and no incentives were provided to the respondents. The data was collected using self-administered semi structured questionnaire and Hospital Anxiety and Depression Scale which was developed by Zigmond and Snaith in 1983 and has 14-item, self-report questionnaire. The tool is valid for screening for anxiety and depressive disorders in non-psychiatric units such as medical and surgical wards; gynecology and antenatal clinics of a teaching hospital and community settings. The self-administered semi structured questionnaires were distributed to the participants and were later collected. A 100% response rate was achieved despite having some missing values. Data was analyzed electronically. Frequencies and percentages were computed for categorical and dichotomous variables. A superimposed normal curve supported with Shapiro Wilk test was used to determine the normality of “age” (continuous variable) which was found not to be normally distributed (p<0.05), thus a reporting was done using the median and interquartile range (IQR). A Kruskal-Wallis or Ranksum test was used to measure the association of age and the outcome variables (counselling and anxiety status). Furthermore, to determine the association between categorical variables, a Chi-square or Fisher's exact test was used (if the expected values in the contingency cell were less than five, a Fisher's exact test was used; otherwise, a Chi-square test was preferred). A Multivariable Logistic Regression Model was used to determine the predictors of counselling. The likelihood ratio test, Akaike's Information Criteria (AIC) and Bayesian Information Criteria (BIC) were used to come up with the best model. A P-value of < 0.05 was considered statistically significant.
RESULTS
Socio-demographic characteristics of health practitioners and Anxiety status
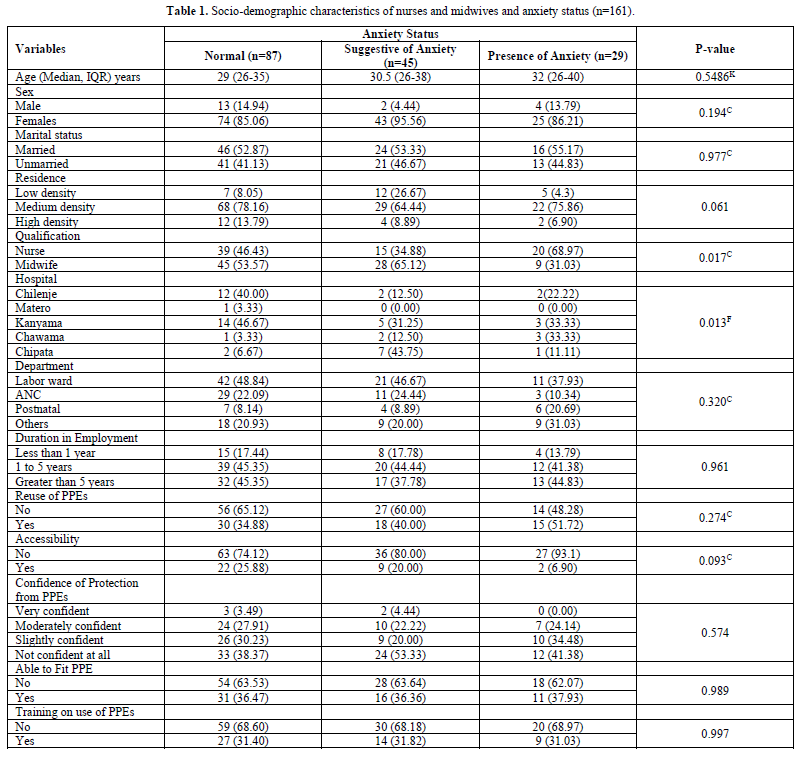
The study had a total population of 167 nurses and midwives from five health facilities. However, only 58 (34.7%) of the respondents indicated their health facility with the following distribution; Matero 1/58 (1.72%), Chilenje 17/58 (29.31%), Kanyama 23/58 (39.66%), Chawama 6/58 (10.34%) and Chipata 11/58 (18.97%). The study reported a median age of 29 (IQR; 26-35) years, 30.5 (IQR; 26-38) and 32 (IQR; 26-40) for those normal, suggestive anxiety and presence of anxiety respectively. However, there was no evidence of statistical significance (p>0.05). Furthermore, the study revealed that 85.06% (74/87) of female respondents had normal anxiety status compared to males, 95.56% (43/45) of females had suggestive anxiety compared to males and 86.21% (25/29) of females had presence of anxiety compared to males (Table 1). The study reported that 53.57% (45/84) and 65.12% (28/43) of midwives had normal and suggestive anxiety status respectively compared to nurses. However, 31.03% (9/20) of midwives had presence of anxiety compared to nurses. In relation to study setting, Chilenje and Kanyama 1st level hospitals reported the highest normal anxiety percentages compared to other hospitals. Suggestive anxiety was high in Kanyama (31.25%) and Chipata (43.75%) whereas presence of anxiety was high in Kanyama (33.33%) and Chawama (33.33%). The findings further show that qualification and hospital were significantly associated with anxiety with a P value of 0.017 and 0.013 respectively (Table 1).
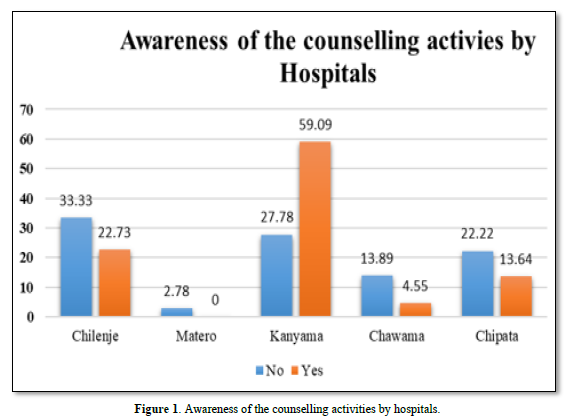
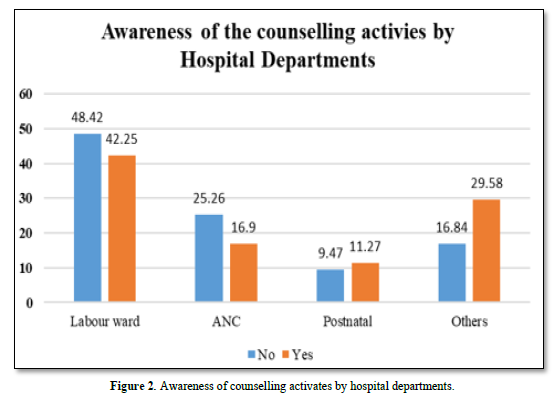
Availability of counselling centers
The study showed that only 42.51% (71/167) of the respondents were aware about the availability of counselling centres in the facilities which was distributed as Chilenje, 29.41% (5/17), Matero, 0%, Kanyama, 56.52% (13/23), Chawama, 16.67% (1/6) and Chipata, 27.27% (3/11). Furthermore, those who were aware of the counselling centres in their health facilities, 42.25% (30/76) were working in the labor ward, 16.9% (12/36) were in Antenatal Clinic, 11.27% (8/17) and 29.58% (21/37) were working from Postnatal and other departments as shown in Figures 1 & 2 below.
Socio-demographic characteristics of nurses and midwives who received counselling
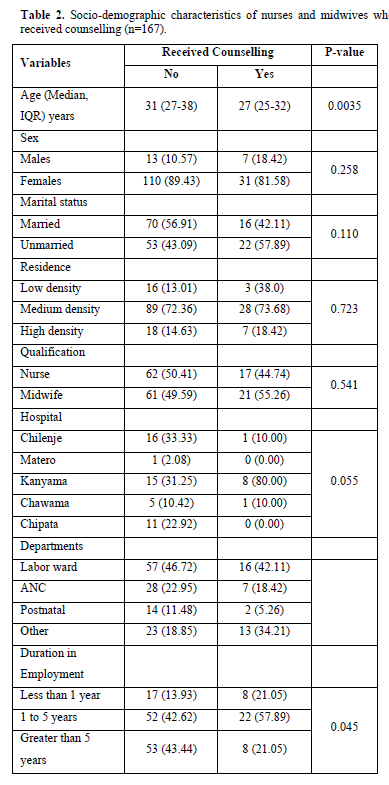
Table 2 below shows the baseline characteristics of participants who received counselling. The mean age of participants who received counselling was 27 (IQR; 25-32) years compared to those who never received did, 31 (IQR; 27-38) years. There was sufficient evidence of a difference (P=0.0035). The findings also revealed that 81.58% (31/38) of female participants received counselling compared to 18.42% (7/38) males, however there was no evidence of a difference between the two. The study further shows that 57.89% (22/38) of those who had been in employment for 1 to 5 years had received counselling compared to 21.05% for both those with less than 1 year and greater than 5 years employment duration. The results show evidence of a difference in the utilization of counselling.
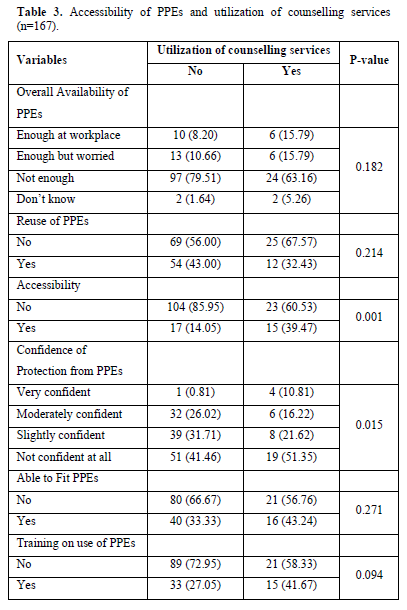
Accessibility to PPEs and utilization of counselling services
The study shows that 60.53% of those who never accessed PPEs utilized counselling services more than those who accessed (39.47%) p value = 0.001. Similarly, those who reported not confident and slightly confident in the use of PPEs (51.35% and 21.62% respectively) had utilized counselling services more than those who reported moderately confident (16.22%) and very confident (10.81%). The findings further show that accessibility to PPEs was significantly associated with confidence of protection from PPEs (P value 0.015) Table 3.
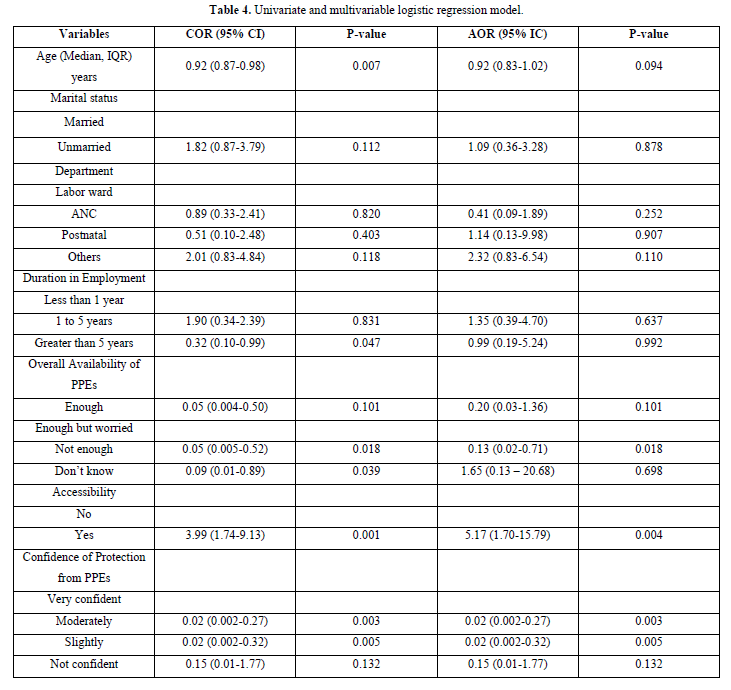
Univariate and Multivariable Logistic regression
The results in Table 4 below shows the univariate and multivariable logistic regression model on utilization of counselling services in the health facilities. Controlling for other factors a year increase in the age of nurses and midwives reduced the odds of utilization of counselling services by nurses and midwives (AOR, 0.92; 95% CI, 0.83-1.02; P<0.094), however there was no evidence to suggest an association. Nurses and midwives who reported the availability of PPEs had reduced odds of utilizing counselling services compared to those who reported not enough (AOR, 0.13; 95% CI, 0.02-0.71; P=0.018), holding all factors constant. Furthermore, the findings show that the nurses and midwives who had access to PPEs had increased odds of utilizing counselling by a factor of 5.17 times (95% CI, 1.70-15.79), controlling for all other factors. Nurses and midwives who were moderately confident in the protection of PPEs had reduced odds of utilizing counselling services following Covid-19 exposure compared to those who reported to be very confident (AOR, 0.02; 95% CI, 0.002-0.27; P=0.003), controlling for other factors. Similarly, those who reported to have slightly confident on the protection of PPEs had reduced odds of utilization of counselling holding all factors constant. Confidence in the protection of PPEs, accessibility and availability of PPEs was significant (P<0.05) in the multivariable model, however in the univariate model age, duration of employment, confidence in the PPEs, availability and accessibility of PPEs was as well statistically significant (P<0.05). The results were first run in the mixed effect logistic regression and the variance found was zero, which suggested that we did not have to worry about intra-cluster variance. To select the best model from competing models, the investigator led was used supported by the AIC and BIC. The likelihood ratio test from the best-fit model also suggested that this model was better than the null model (P<0.0001).
DISCUSSION OF FINDINGS
The study participants comprised of nurses and midwives from the Women and New born Hospital and five first level hospitals (Matero, Chilenje, Kanyama, Chawama and Chipata) in Lusaka, Zambia. The study was conducted to determine the anxiety and utilization of counselling services among the nurses and midwives during the COVID-19 pandemic. Anxiety was measured in three categories namely normal anxiety, suggestive of anxiety and presence of anxiety.
Socio-demographic characteristics of health practitioners and Anxiety status
The study reported a median age of 29 (IQR; 26-35) years, 30.5 (IQR; 26-38) and 32 (IQR; 26-40) for those with normal, suggestive anxiety and presence of anxiety respectively. This shows that older nurses and midwives had presence of anxiety compared to younger ones although there was no statistical significance of this association. These findings are contrary to findings of descriptive correlational study conducted to determine anxiety levels and solution-focused thinking skills of nurses and midwives working in primary care during the COVID-19 pandemic in which overall, all participants' anxiety scores were above average, indicating a moderate level of anxiety [11]. According to the findings of other recent studies, the healthcare workforce has faced high levels of anxiety since the COVID-19 pandemic. This anxiety could be due to the infectious nature of the disease and fear related to acquiring the infection, spreading it to family members later or fear of death. In this study, more female participants had normal anxiety status, suggestive anxiety and presence of anxiety compared to male respondents. This finding is similar to findings of a study conducted to evaluate the level of health anxiety in nurses caring for patients with COVID-19 which showed higher levels in female nurses caring for patients with COVID-19 compared to males. A nationwide cross-sectional survey conducted to determine the depression, anxiety and stress during COVID-19 pandemic among midwives in Ethiopia reported similar findings. Females are more predisposed to anxiety and mood disorders due to genetic, biological, hormonal, social and psychological factors. On the contrary, androgen receptors in men give them protection and resilience to stand stressful situations. Additionally, various stressors including role pressure, difficulty in balancing work life, and inadequate support uniquely affect females. It is expected that the psychological distress increased during the COVID-19 pandemic among female nurses and therefore contributing to this picture of higher numbers of female nurses presenting with anxiety than males. This study showed that qualification and the research setting were significantly associated with anxiety with a P value of 0.017 and 0.013 respectively. The findings revealed that 53.57% (45/84) of midwifes had normal and suggestive anxiety status compared to nurses, 65.12% (28/43). The anxiety experienced by both nurses and midwives could be due to perceived high risk of getting the infection due to exposure to the infections as they attended to patients. Anxiety could be due to fear of being infected and infecting their loved ones back home. Additionally, it is difficult to maintain physical distance during care provision. The exposure is even more for midwives as most perinatal care visits require prolonged contact time with clients. Inadequate supplies of PPEs in the facilities could also heighten the anxiety among nurses and midwives. Similarly, a library review study conducted to investigate the relationship between the prevalence of COVID‐19 and nurses' anxiety disorder reported that nurses had a mental health breakdown and became very anxious during the COVID‐19 due to fear of infection when providing close-contact care to patients infected with COVID-19. According to studies in Iran, the causes of anxiety among care provider caring for COVID-19 patients were fear of being infected, the difficulty of controlling the pandemic and lack of medical equipment. Additionally, on the facilities that had nurses and midwives presenting with anxieties, Chilenje (40%) and Kanyama (46.6%) first level hospitals reported the highest normal anxiety percentages compared to other hospitals. Suggestive anxiety was high in Kanyama (31.25%) and Chipata (43.75%) whereas presence of anxiety was high in Kanyama (33.33%) and Chawama (33.33%). All these first level hospitals are government owned, highly populated and most often with inadequate supply of PPEs. Another challenge faced by public or government hospitals is the shortage of nurses and midwives, which in turn leads to increased workload and worsens the anxieties among nurses and midwives. These findings are similar to that of a study conducted to determine the levels of depression, anxiety and stress, during COVID-19 pandemic among midwives in Ethiopia. The study reported that midwives who worked in government hospitals were more likely to experience anxiety compared to those that worked in the private hospitals. This could be attributed to non-availability and accessibility of the PPEs, which puts the nurses and midwives at risk of contracting the COVID 19. Similarly, participants of a study conducted to explore the challenges, strategies, and outcomes of stress management in nurses who faced and provided care to COVID-19 patients cited lack of personal protective equipment and coveralls, particularly in the early days of the pandemic, as one of the main obstacles to stress management [13-20].
Availability of counselling centers
This study revealed that less than half of the respondents 42.59% (69/162) were aware about the availability of counselling centers in the facilities. Most (56.52%), of the respondents who were aware of the availability of counselling services were from Kanyama while none (0.00%), of the respondents from Matero 1st level hospital was aware of the availability of counselling services. The study further showed that most 68.57% (24/35) of the respondents who were aware of the counselling center in their health facilities were working in antenatal clinic, while the least, 39.19% (29/74), were working in the labor ward. Availability of counselling services is cardinal in helping nurses and midwives cope with anxiety because of caring for COVID -19 patients. However, this lack of awareness of counselling services would lead to lack of utilization of counselling services by nurses and midwives caring for COVID-19 patients. A study conducted to explore the challenges, strategies, and outcomes of stress management in nurses who face and provide care to COVID-19 patients recommended that nurses who are directly involved in providing care for COVID-19 patients should take steps to reduce stress and anxiety. Such measures include seeking counselling from a psychologist, as persistent anxiety can result in psychological distress, depression, and other problems [20].
Nurses and midwives who received counselling
Nurses and midwives were overwhelmed by the COVID-19 pandemic amidst the frontline roles they played during the pandemic. The pandemic took a toll on nurses and midwives both physically and psychologically as nurses witnessed numerous deaths, which left them traumatized as well as scared of possible infection. Nurses and midwives therefore needed strategies to deal with these challenges and anxieties. Counselling services could be such strategies to help nurses and midwives cope with these stressors. This study showed that younger participants received counselling, median age 27 (IQR; 25-32) years compared to older participants 31 (IQR; 27-38) years. Age was significantly associated with receiving counselling services with a p value of 0.0035. The older one grows, the higher the chances of developing positive help-seeking attitudes. This study further revealed that more female participants 81.58% (31/38) received counselling compared to males 18.42% (7/38), although there was no statistical significance. Further, the study showed that more (57.89%) participants who had been in employment for at least 1 to 5 years received counselling compared to 21.05% for both those with less than 1 year and greater than 5 years in employment with a p value of 0.045. A scoping review conducted to investigate the nature of work related with psychosocial challenges nurses encountered during the peak of the pandemic and the coping strategies recommended regular counselling and support for all nurses working at the frontline to help them better handle with the devastating effects of the pandemic so that they could build resilience towards future pandemics [21]. Another study pointed out that the nurses could adopt several coping strategies to overcome their distress. Such strategies include self‐care management which involves using spiritual coping, physical exercise, and yoga. Self‐care is essential for nurses as a lack of it during times of stress will affect their ability to provide care and increase anxiety levels [22].
Accessibility to PPEs and utilization of counselling services
This study showed that participants who did not access PPEs utilized counselling services more than those who accessed (39.47%). Univariate and Multivariable Logistic regression showed that nurses and midwives who reported the availability of PPEs had reduced odds of utilizing counselling services compared to those who reported not enough (AOR, 0.13; 95% CI, 0.02-0.71; P=0.018), holding all factors constant. Nurses and midwives who were moderately confident in the protection of PPEs had reduced odds of utilizing counselling services following COVID-19 exposure compared to those who reported to be very confident (AOR, 0.02; 95% CI, 0.002-0.27; P=0.003), controlling for other factors. The PPEs for healthcare personnel particularly nurses and midwives is an essential part of infection prevention and control. Protecting nurses and midwives from infection results in more effective infection containment [23]. Utilization of PPEs gives reassurance and protection from contracting the infection. As such, participants who accessed and utilized PPEs were less worried about contracting the infection and so did not seek counselling. The study further showed that accessibility to PPEs was significantly associated with confidence of protection from PPEs (P value 0.015). Participants who utilized PPEs during the pandemic felt less vulnerable of contracting the infection and so were less likely to be anxious nor seek counselling services [24-29].
CONCLUSION
The current study has demonstrated that the COVID-19 pandemic increased anxiety levels among nurses and midwives providing care in maternity settings of the five Lusaka hospitals in Zambia. These frontline workers need support in terms of counselling services in order to help them cope with stressful event of care giving. Availability of PPEs also played a major role in reducing the psychological stress that was due to care giving during the COVID-19 pandemic.
No Files Found
Share Your Publication :