-
Publish Your Research/Review Articles in our High Quality Journal for just USD $99*+Taxes( *T&C Apply)
Offer Ends On
Levy Pinto*, Edma Sulemane and Luís Mouliaá
Corresponding Author: Levy Pinto, Department of Physical Medicine and Rehabilitation, Maputo Central Hospital, Mozambique.
Received: August 08, 2022 ; Revised: August 27, 2022 ; Accepted: August 30, 2022 ; Available Online: November 08, 2022
Citation: Pinto L, Sulemane E & Mouliaá L. (2022) Perceived Barriers and Facilitators for the Practice of Physical Exercise by People with Spinal Cord Injury in Maputo-Mozambique. J Ageing Rehab Res, 1(2): 1-9.
Copyrights: ©2022 Pinto L, Sulemane E & Mouliaá L. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Views & Citations
Likes & Shares
Background: People with activity limitations, such as spinal cord injury, are more likely to lead a sedentary lifestyle. Physical exercise and sport programs are an effective strategy for promoting rehabilitation in a broad sense of the term, as it accelerates the rehabilitation process by promoting: physical and health improvements, psychological gains, social inclusion, resulting in increased quality of life.
Objective: This study sought to know the barriers and facilitators perceived by people with spinal cord injury for the practice of physical exercise in Maputo city.
Methods: This is qualitative research, with semi-structured interviews carried out with 26 people with spinal cord injury, using thematic analysis as a methodological tool.
Results: Most participants reported that, before the spinal cord injury, they practiced physical exercises either at home, outdoors, gyms and expressed an interest in becoming active or maintaining an active lifestyle. Several barriers were identified for the practice of physical exercises: accessibility to sidewalks, gyms, fields, bathrooms; lack of public transport; distances traveled to find a gym, field; reliance on third parties to get around; lack of specific personnel to train them and fear of injuries. All participants think positively about physical exercise, associating it with well-being, health, social interaction, improved functionality in general, prevention of secondary conditions such as pressure ulcers.
Conclusion: People with spinal cord injury face several barriers to physical exercise. The removal of these barriers, associated with the promotion of facilitating factors, is crucial to improve the opportunities for people with spinal cord injuries to practice physical exercises and reduce the risk of costly secondary conditions in this population group.
Keywords: Barriers, Facilitators, Exercises, Spinal cord injury
BACKGROUND
Spinal Cord Injury (SCI) is a devastating neurological event that changes the life of the affected person, with an impact not only on the individual, but also on the people closest to him, namely family members and caregivers [1-4].
Studies indicate that the person with SCI becomes sedentary, has a high lipid index, has limited independence, tends to have low self-confidence, has loss of muscle mass, has respiratory and cardiovascular problems, premature aging among many other factors harmful to your health and wellbeing [5-10].
Physical exercise has been shown to decrease the risk of many of the secondary conditions associated with SCI, including osteoporosis, cardiovascular disease, pressure ulcers, urinary tract infections, diabetes, and arthritis, although this population is rarely targeted by health promotion efforts [9,11].
Upon returning to the community after rehabilitation, people with activity limitations, such as SCI, are less likely to be physically active compared to the non-disabled population [12].
Health promotion for people with disabilities (PwD) has been a neglected area of interest by the health community in general. The goals of a health promotion program for PwD are to reduce secondary conditions (e.g., obesity, hypertension, pressure ulcers), maintain functional independence, provide an opportunity for leisure and fun, and improve the overall quality of life by reducing environmental barriers to good health [6].
Little has been investigated about why most people with disabilities are unable to integrate regular physical activity into their lifestyle. Understanding the likely barriers and facilitators that affect the participation of these people could provide important and necessary information for the development of interventions that are more likely to be successful [9,13].
The justification for the study was based on the scarcity of specific information on barriers and facilitators for the practice of physical exercise by people with SCI in Mozambique, and considering that this information is essential for the development of effective interventions that contribute to improving lives. of people with disabilities, being a new, important and interesting study. Therefore, its relevance is centered on contributing to the definition of adequate strategies (based on evidence) for the formulation of plans and public policies to be adopted by official entities, researchers, health professionals, physical education professionals, advocates and volunteers involved with the disability issue with a vision of a world of inclusion and contribute so that everyone is able to live a life of health, comfort and dignity by increasing participation in physical exercise programs after SCI.
In view of the above, the objective of this study was to identify the perceived barriers and facilitators for the practice of physical exercise by people with SCI in Maputo city.
METHODOLOGY
We carried out a cross-sectional study of an exploratory and descriptive nature through semi- structured interviews. The treatment and interpretation of data were carried out based on thematic analysis. The study involved 26 people with SCI, followed at Physical Medicine and Rehabilitation services and living in Maputo. Participants were selected by convenience. For the inclusion criteria, we applied: people with SCI of any etiology, with more than one year of evolution, aged 18 years or over and who agreed to sign the informed consent form. Data collection took place in March and April 2022.
The data collection instrument consisted of three parts: the first part was socio-demographic information with data characterizing the subjects and identification variables; the second part clinical information/injury data and closed-ended questions; the third and last part was a questionnaire related to physical exercise. The data collection instrument was tested by 5 people with SCI.
Although most existing post-SCI exercise research has been conducted in a controlled setting, through a structured exercise program, using a number of standardized means to measure exercise, including a structured reporting scale [14,15], a validated self-report instrument [16], an activity monitor [12] or providing exercise parameters to use for self-identification (e.g. 30 minutes a day, etc.) [17], in contrast, this study took into account the individual's perception of physical exercise and not pre-defined categories.
Consequently, in this article, we will use the term exercise to refer to both formalized exercise activities and physical activity performed at home. This understanding of exercise reflects the recommendation by the Centers for Disease Control and Prevention and the American College of Sports Medicine that both low-intensity activity and vigorous exercise are beneficial in reducing the risk of heart disease and increasing overall fitness levels (USDHHS: Physical activity and health APUD Kehn and Kroll) [9].
Each interview lasted an average of 30 minutes and the answers were recorded in the interview script. After a thorough reading of the interview scripts, the speeches of the study participants were subjected to thematic analysis. To preserve anonymity, the interviews were coded, we used the letter E followed by a number to identify the participants' statements.
We respect all ethical aspects throughout the study and the protocol was approved by the Institutional Committee on Bioethics in Health of the Faculty of Medicine/Maputo Central Hospital (CIBS FM & HCM) under the number CIBSFM & HCM/102/2021.
RESULTS
Socio-demographic and clinical characterization of study participants
Although we do not work with generalizations, we found that the participants are distributed in a wide age group between 20 and 63 years old. The mean age of participants was 39 (±17) years. Most participants were aged between 31 and 40 years (n=9) (Figure 1).
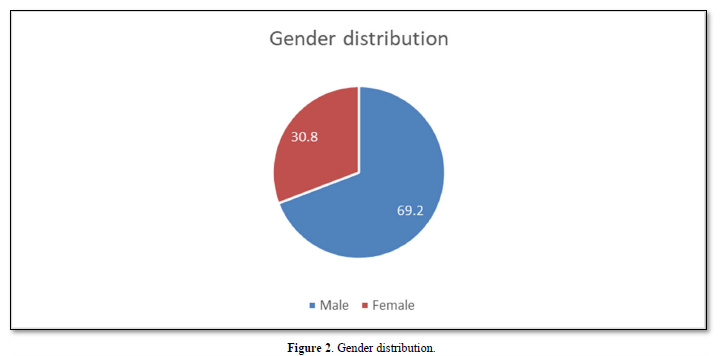
Regarding gender, 69.2% were male and 30.8% were female (Figure 2). Most participants were paraplegic (17/65%), with trauma as the main cause of injury with 65.4% (Figure 3). When analyzing the group of traumatic injuries, most were caused by a road accident with 64.7%. Regarding non-traumatic causes, 66.7% were caused by Pott's disease.
Experience in relation to physical exercises before SCI
Before SCI, most of the study participants (76.9%) reported that they practiced physical exercises whether outdoors, at home, in gyms or sports fields, as reported below:


The word physically active was used in the participants' discourse to express the perception of physical exercise.
Experience of physical exercise after SCI
However, not all pre-injury exercisers continued to exercise after injury and some pre-injury non- active participants became active after SCI. Of the participants who reported physical activity before the injury, only 6 reported physical exercise after the injury and of those who did not report physical exercise before the injury, 3 reported physical exercises after the injury.
Some study participants stopped exercising due to injuries or complications associated with their condition, or other priorities. The interviews conducted revealed a wide range of factors that were identified as impediments for individuals with SCI to become physically active and prevent secondary conditions.
The thematic analysis identified four main factors acting as barriers and perceived facilitators for the practice of physical exercises: environmental, social, personal and structural or process factors (Table 1).
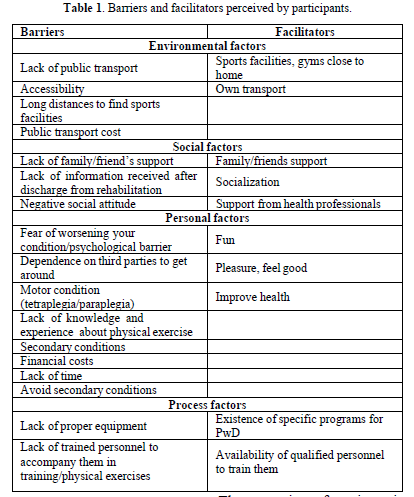
Environmental factors
As reported by the participants, several barriers related to the environment were reported: lack of transport to go to training camps, long distances to access a field, gym, accessibility to public spaces, including access to bathrooms.
The transcripts of our interviewees below reveal the barriers described above:
As facilitators, the fact that they have their own transport and drive their own car and the proximity of a field, gym, were reported.
Social factors
Of these, it is worth highlighting the lack of information received from professionals after discharge from rehabilitation, lack of family/friend’s support, negative social attitude as follows in the following speeches:
Three of the participants made comments that dictate the behavior of society, that it is not prepared or has completely wrong attitudes when we think of someone with a disability:
Among the social facilitators, support from family and/or friends, encouragement from health professionals, socialization.
Personal factors
Several factors were mentioned as personal barriers to the practice of physical exercises: dependence on others to get around, fear of worsening health/psychological barrier, neuromotor condition (quadriplegia or paraplegia), lack of knowledge and experience about physical exercise, lack of time, lack of money to pay for a gym/economic cost. Physical aspects that were mentioned as barriers to the practice of physical exercises included having an injury or a complication associated with the condition and tiredness.
Another factor considered as a barrier to the practice of physical exercise was lack of time.
Most participants, who exercise reported doing so to prevent secondary conditions, particularly pressure ulcers, urinary tract infections and muscle wasting, as well as improve bowel movement. Regarding the facilitators, the participants mentioned the taste for physical exercises, fun, pleasure, avoiding secondary conditions caused by a sedentary lifestyle, according to the following reports:
Another aspect said to facilitate was the control of intestinal transit:
Process or program factors
When we look at process or program related factors, we refer to organizational issues such as specific programs, trained personnel, adequate equipment, etc.
According to the reports of the study participants, the barriers mentioned were the lack of trained personnel to accompany them and the lack of adequate equipment.
Regarding the facilitating factors, mention should be made of the existence of specific programs and trained personnel.
Perceived health benefits of physical exercise
The result of the study showed that all individuals think positively about physical exercise, associating it with well-being, health, social interaction, improvement of functionality in general, prevention of secondary conditions such as pressure ulcers.
Other benefits were observed in relation to general cardiovascular and respiratory fitness. Being physically active was also seen as improving motor control and maintaining strength.
As we see in the testimonies, there is a common feeling in relation to the positive effect of physical exercise on health: preventing injuries, improving quality of life, improving agility, avoiding cardiovascular problems and providing psychological well-being.
PwD constitutes a somewhat strategic group on the global agenda, aiming at their full and effective participation in society and on an equal basis with others.
This qualitative study showed that there are several factors including environmental, social, personal and process that can be a barrier or facilitator for people with SCI to remain physically active. Some barriers found are not specific to people with SCI but found in the general population.
The main environmental barriers perceived for the practice of physical exercises were: the problem of public transport, accessibility and the lack of sports infrastructure in all rural and urban environments. This finding is consistent with a study carried out in the Western Cape province of South Africa where lack of transport, followed by accessibility issues and lack of sports infrastructure in all environments were the main barriers identified [17].
The issue of accessibility was also reported in a study developed by the Rehabilitation and Research Training Center (RRTC) on Spinal Cord Injury [9].
Maputo city has serious public transport and accessibility problems. This problem largely affects PwD and in particular people with SCI who depend on their wheelchairs to get around.
It is evident that there is a permanent imperative to strengthen policies aimed at reducing barriers in the physical environment and incorporating universal design principles for the benefit of all users [18].
The location of sports facilities or the location where programs are offered also plays a role as a barrier to individuals with SCI becoming physically active. However, the lack of transport contributes to the problem.
The identification of environmental barriers, especially those related to accessibility, are not exclusive to the problem of physical exercise, and were reported in conjunction with access to health services [9].
When we look at environmental facilitators, our results refer to the proximity of their homes to sports facilities and the fact that they are independent, having their own transport. The ease of finding a sports infrastructure as a facilitating factor was also reported by a study carried out in South Africa [17].
As for social barriers and facilitators, our results do not differ from the results found in other studies.
One of the barriers reported in our study was the lack of information regarding sport after the injury. This finding is consistent with a study by Malone et al. [19] where he found that people with physical disabilities do not receive adequate information regarding sport.
Limited family and social support have also been reported in studies as a barrier to the practice of physical exercise by people with SCI [20].
As for the facilitators, the literature consulted reports that sport is a powerful tool for the person's reintegration into social life, in addition to providing good mood, increasing self-esteem, expanding the cycle of friendships, happiness and joy to continue in the fight for the achievement of your space [21].
The support of family, friends and the behavior of the professional responsible for promoting physical exercise are important facilitating factors for people with motor disabilities to become physically active [14].
Socialization and the increase in the cycle of friendships were reported in other studies as facilitators for the practice of physical exercises, in Kenya [22] and the Netherlands [23].
Regarding personal barriers, our findings are consistent with the literature consulted [12,17,24]. Secondary conditions are often the cause of re-hospitalizations, subsequent bed rest and physical inactivity. It is important that these barriers are eliminated to improve the health and well-being of people with SCI [24].
Lack of time and financial conditions were also reported as barriers for people with SCI to become physically active [25].
Regarding perceived personal facilitators, they also coincide with what is found in the literature in which feeling good, having fun and improving skills were reported [17].
When we look at the process barriers reported here, the lack of trained staff to monitor, the lack of accessible gyms both in terms of architecture and financial costs and the lack of specific programs, these findings were also reported in other studies.
In the literature consulted, we found the cost of exercise programs as a barrier [19]; lack of experience of staff working in gyms in caring for people with SCI [26] and lack of adequate equipment for people with SCI [27].
As facilitators, the fact of having specific programs with trained personnel to accompany them and the existence of adequate equipment was also found in other studies [9,17].
Being a person with a disability is not just about medical issues, but more importantly social and inclusion issues [28].
Regarding the perceived benefits of physical exercise, our findings coincide with those found in other studies [10,19]. Physical exercise improves general health, well-being and prevents secondary conditions, especially pressure ulcers, in addition to improving circulation, breathing, and agility.
STRENGTHS AND LIMITATIONS
This is the first study that deals with barriers and facilitators for the practice of physical exercises perceived by people with SCI in Maputo-Mozambique. However, some limitations of the study were found. Its qualitative nature does not allow the results to be generalized to a larger population. The methodology used does not allow conclusions to be drawn about which barriers and facilitators have the greatest impact. Another limitation of this study was the fact that we used individual perception in relation to physical exercise and not pre-defined categories.
IMPLICATIONS
The results of this study provided an overview of the main barriers and facilitators for the practice of physical exercises perceived by people with SCI in the city of Maputo that can contribute to the elaboration of a multisectoral plan to promote the participation of PwD in general in the practice of physical exercises.
It can also serve as a baseline for future quantitative studies with larger samples evaluating associations between different barriers (personal, social, environmental and process) and physical exercise in this population. It is important that this study be replicated at both rural and urban levels, taking into account the differences between them. The present study can also be replicated in people with other types of disabilities.
CONCLUSION
Based on the results of the study, it is evident that there are several barriers and facilitators perceived by people with SCI for the practice of physical exercises. The barriers encountered are multiple and result from a combination of environmental, social, personal and process factors.
Among the barriers found the lack of public transport, accessibility, lack of family and/or friends support, dependence on third parties stand out. Accessibility does not refer only to the sports environment, but also to other social spaces, which is a right that has not been guaranteed. Socialization, improved functionality in general and improved quality of life was mentioned as facilitators.
The removal of these barriers, associated with the promotion of facilitating factors, is crucial to improve the opportunities for people with SCI to practice physical exercises and reduce the risk of costly secondary conditions in this population group.
When physical inactivity is not addressed within people with SCI, health and well-being are not achieved, quality of life is affected and affected individuals are predisposed to many other comorbidities and secondary health conditions.
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
AUTHORS' CONTRIBUTIONS
LP was the principal investigator of this study and involved in the original protocol design. LP, ES and LM developed the semi-structured interview guide together.
All interviews were conducted by LP. Interview transcriptions, subsequent analysis and development of this manuscript were performed by LP and ES. All authors approved this final manuscript.
FUNDING
The authors did not receive any financial assistance in support of the study.
ACKNOWLEDGMENTS
We sincerely thank the study participants who shared their perceptions with us and gave us their consent to publish this work.
No Files Found
Share Your Publication :