-
Publish Your Research/Review Articles in our High Quality Journal for just USD $99*+Taxes( *T&C Apply)
Offer Ends On
Shakina Bellam, Rohini Ravishankar, Mamta Kumari, Rachel Steele, Anne Aboaja and Amanda E Perry*
Corresponding Author: Amanda E Perry, University of York, Department of Health Sciences, ARRC Building, Heslington, York, YO10 5DD, UK
Received: April 06, 2022 ; Revised: April 24, 2022 ; Accepted: May 7, 2022 ; Available Online: May 20, 2022
Citation: Bellam S, Ravishankar R, Kumari M, Steele R, Aboaja A, et al. (2022) Psychological Interventions to Reduce Gambling Behavior Among People Involved in the Criminal Justice System: A Systematic Review and Recommendations. J Psychol Psychiatry Res, 1(2): 1-9.
Copyrights: ©2022 Bellam S, Ravishankar R, Kumari M, Steele R, Aboaja A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Views & Citations
Likes & Shares
Abstract
Background: People involved in the criminal justice system are at an elevated risk of developing problem gambling. Despite this, the effectiveness of treatment interventions to reduce gambling behavior in this population are largely unknown. We conducted a systematic review and propose recommendations for future research.
Methods: We systematically reviewed MEDLINE, PsycINFO and Embase and grey literature following Cochrane Collaboration guidelines between 2005 and March 2020. We identified psychological interventions of randomized controlled trials and quasi-experimental studies for people involved with the criminal justice system with gambling problems. Data were extracted on the primary outcome of gambling behavior, and secondary outcomes of self-harm, suicidal behavior, alcohol, drug misuse and quality of life measures. We conducted a narrative synthesis and used the Cochrane risk of bias and the Joanna Briggs Inventory tools to assess methodological quality.
Findings: Our search yielded 759 records. 42 full text articles were assessed for eligibility, two randomized controlled trials and one quasi-experimental study involving 684 people met the inclusion criteria. Interventions included a brief referral system, cognitive behavioral therapy and a prison-based psychoeducational program. None of the treatments were found to be superior to the alternative comparison. Outcome measures of problem gambling were varied, no secondary outcomes were reported. Methodological quality varied across the studies.
Interpretation: Research to identify effective interventions to reduce gambling behavior in criminal justice involved populations are needed. Evidence to address questions relating to the impact of initiated treatment effectiveness. A public health framework is required to develop the co-production and adaptation of existing interventions to increase motivation, uptake and consider the comorbidity between physical and mental health and gambling behavior. Collaborative agency work is required to develop new pathways for treatment.
Keywords: Gambling, Systematic review, Criminal justice, Offenders
INTRODUCTION
Between 9 million and 444 million individuals are known to suffer from problem gambling worldwide [1]. In the UK more than 2 million people are either ‘problem gamblers’ or at risk of addiction [2]. Research suggests that individuals involved in the criminal justice system (CJS) have an e0levated risk of experiencing gambling problems in comparison to those with no CJS contact [3-8]. Although Gamblers Anonymous remains a popular approach, it typically attracts older, married and high-income clients that are unlike the majority of people involved in the CJS [9]. The estimated societal costs incurred by problem gamblers are considerable [10] and there have been recent calls for problem gambling to be recognized as a public health concern [11-14].
Mental health problems such as depression, anxiety co-exist in severe forms of gambling [15-17]. Gambling disorders share many features of other addictive behaviors (e.g., alcohol or drug use) and are often associated with young single men of low socio-economic status [18]. People with current suicidal thoughts, emotion dysregulation, and trait impulsivity reported more severe problem-gambling disorders compared to those without [19-21]. Disordered gambling and the relationship to crime is complex and often involves a range of criminal offences [7,22,23] having a significant impact on individuals, families, cultural groups, employers and society at large [8,24,25].
Meta-analyses of psychological interventions in community populations suggest that cognitive behavioral therapy (CBT), brief in-person individual psychosocial interventions programs [26] and use of motivational interviewing are amongst the most efficacious [27,28]. However, the effectiveness interventions for those involved in the CJS remains unclear [23]. Qualitative studies and pre- and post-test studies with no comparable control groups have been conducted, but high-quality research on the effectiveness of treatment outcomes is required [29-31]. Schemes in the USA court system, lack evidence to support their effectiveness and the potential to cause inadvertent harm and waste of valuable resources is a growing concern [23].
To fulfil this gap, we undertook a systematic review to identify psychological intervention studies to reduce gambling behavior for people involved in the CJS.
RESEARCH IN CONTEXT
Evidence before this study
Gambling is highly prevalent in criminal justice involved populations. Gambling problems are exacerbated through criminal activity and also other psychiatric and psychosocial problems [21,25]. These effects include financial problems, relationship breakdowns and generate a range of health inequalities associated with physical and mental health comorbidities [32].
Added value of this study
This is the first systematic review to identify studies to inform treatment effectiveness to reduce problem gambling behavior for people involved in the CJS.
Implications of all the available evidence
Internationally, only three studies support our current knowledge of how best to treat CJS involved people experiencing problem gambling. A programme of commissioned research is required to address a range of research questions.
METHODS
Search strategy and selection criteria
We searched three electronic databases (MEDLINE, PsycINFO and EMBASE) and grey literature from inception of the UK Gambling Act up until March 2020. The search strategy was developed by an information specialist (RS). Keywords and database specific thesaurus terms were used for all databases including gambling, prison, forensic psychiatry contexts and offending behavior. Synonyms were combined with the Boolean operator OR and different concepts were brought together with Boolean operator AND (Appendix A). No language limits or study design filters were specified. Hand searching of reference lists for included studies and authors of unpublished data were contacted.
Randomized controlled trials (including pilot and cluster randomized) with participants randomized to standard care, (treatment as usual), or another intervention were included alongside quasi-experimental study designs containing a comparable control group. The study population included participants that were incarcerated in prison, jail, secure hospitals, those on parole, probation, in police custody or residing in boot camps, and those with a previous offending history. All participants were adults (aged 18 and over) with a current or past problem gambling diagnosis. We considered interventions that were psychological in nature (e.g., cognitive therapies, motivational interviewing, motivational enhancement therapy, behavioral interventions family therapies and self-help interventions available online). Our primary outcome was any form of reported gambling behavior. Secondary outcomes included self-harm, suicidal behavior, alcohol, drug misuse and quality of life measures. Duplicate studies were removed before title and abstract searching. Authors worked in pairs to screen and extract data from full text papers. Any disagreements were consulted and resolved, when necessary, by independent arbitration (AP). The study protocol was registered with PROSPERO, (CRD42020161876). We follow the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) recommendations for reporting [33].
Data extraction and outcomes
Data on the study population, intervention details and outcome measures for both intervention and comparison groups and outcomes at all follow up points were extracted using a standardized data extraction sheet.
Study quality and risk of bias
Study quality were independently assessed using the Cochrane Collaboration risk of bias tool [34] and the Joanna Briggs Inventory (JBI) Critical Appraisal Checklist [35].
The Cochrane risk of bias tool assesses for seven domains: random sequence generation and allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessors (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other potential sources of bias such as funding to produce an estimate of risk of bias (i.e., low risk, unclear risk or high risk of bias). We did not rate studies on performance bias as the nature of intervention delivery did not allow for blinding of participants.
The JBI critical appraisal checklist assesses bias through nine questions focusing on: the study causal relationship, the existence of a control group, the similarity of people in groups, type of intervention, existence of pre and post-test intervention measures, statistical analyses, follow up and outcome measures on both groups. All items were rated either yes/no or not applicable [35].
Statistical analysis
Due to the paucity of evidence, we were unable to explore heterogeneity using statistical methods (e.g., Q and T2 statistics), nor could we conduct any meta-analysis to estimate the effect size (e.g., Hedges’ g) [36]. Instead, we provide a narrative summary of each study and generate recommendations for research.
Role of the funding source
There was no funding source for this study. The corresponding author had full access to all data and had final responsibility for the decision to submit the publication.
RESULTS
Study characteristics
We identified 759 search results (Figure 1), 663 were screened at the title and abstract level. After duplication, 621 studies were excluded and 42 full text studies were assessed.

A further 39 were excluded for (i) not including an intervention aimed at reducing gambling, (ii) not including CJS populations, and (iii) lacking a comparable control group. Three studies (with five publications) were included in the review [7,37-40].
The total study population included 684 participants. Of those randomized, 236 (34%) were male and 121 (17%) female) [37-40]. The remaining 327 (47%) were male participants assigned in one quasi-experimental study [7]. Among those participants 421/684 (61%) received an intervention, whilst 263 remained in the control or comparison groups. The mean age of the study participants ranged from 32.49(SD 7.27) to 45.8(SD 11.6) years (Table 1). There was no significant difference between the intervention and control groups for gender or age in the included studies. All three studies were conducted in the United States. One study used an incarcerated prison population [7], one study referred participants through a pre-trial probation service [38-39] and the third study was a secondary analysis of a trial that included CJS involved people with a previous offending history [40].
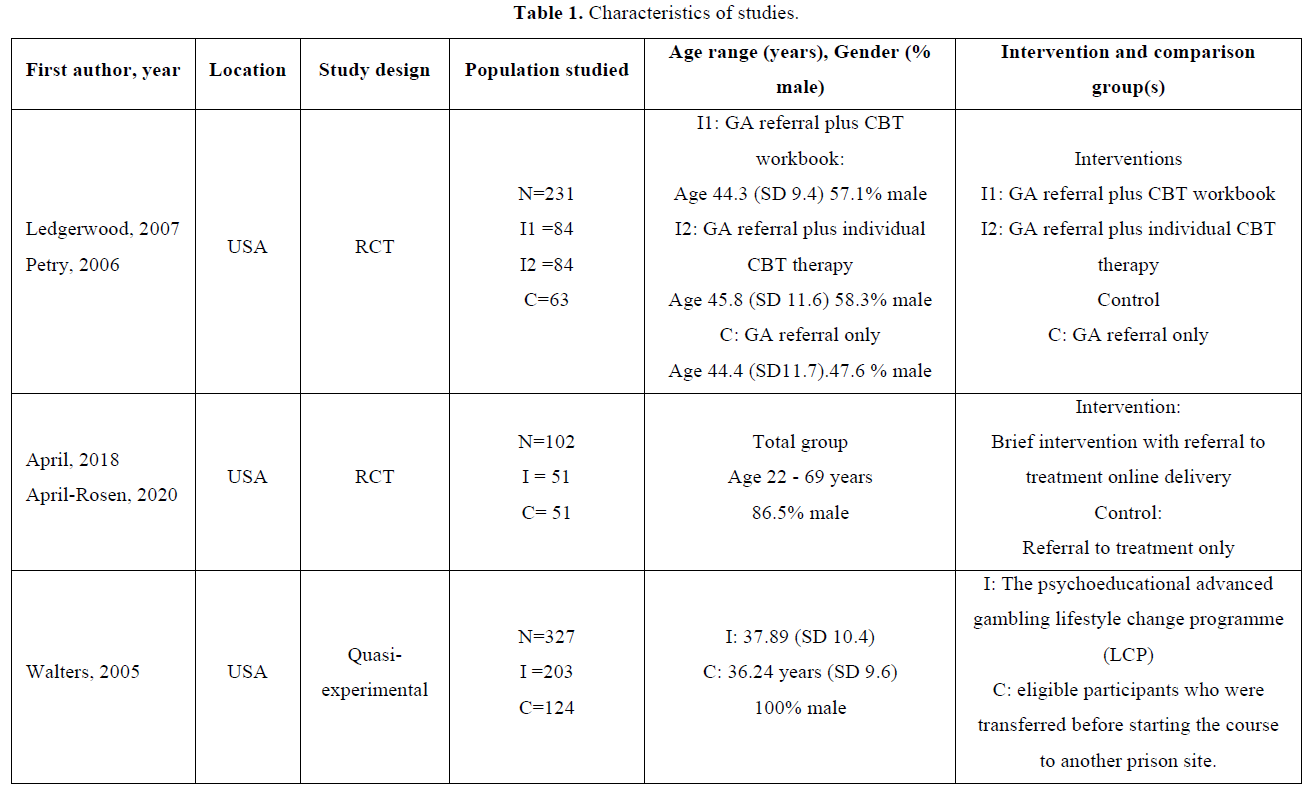
Interventions and outcomes
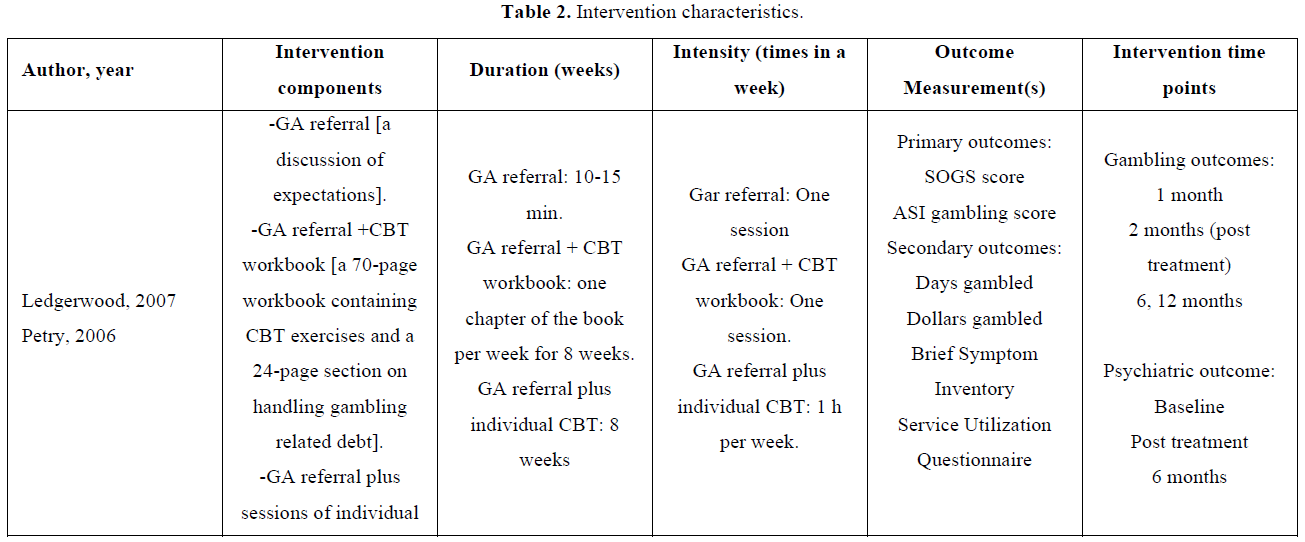
The intervention comparisons included referral to a gambling support group in addition to therapist-led or self-help psychotherapy versus referral to the support group alone [37], referral to treatment with an online gambling intervention versus treatment as usual [39]; and a gambling psychoeducation programme versus no intervention [7]. The intervention durations varied between 1 and 12 months and follow-up assessments were completed at baseline, 1, 2, 5, 6 and 12 months.
Measures of gambling behavior included the South Oaks Gambling Screen (SOGS) score, Addiction Severity Index (ASI) the Addiction Severity Index Gambling Scale (ASI-G), Problem Gambling Severity Index (PGSI), Attitudes Towards Gambling Scale-8 (ATGS-8) and Gambling Treatment Utilization Questionnaire. Other measures of gambling behavior included the number of days and dollars gambled [40] and the total number of disciplinary and gambling related disciplinary reports [7]. No single study reported on our secondary outcome measures, however, one study did report on psychiatric symptoms but were not reported pre and post-test [37-40].
STUDY SUMMARIES
Offenders under the care of the probation and pre-trial service
269 ex-offenders in Southern District of Illinois Probation and Pre-trial Services Office were identified [38,39]. Following pre-screening 102 individuals were randomized using the following criteria: (1) age 18 or older, (2) English speaking, (3) were currently receiving probation, parole or supervised release services within the St. Louis Metropolitan area, and (4) responded correctly to embed validity checks. The mean age of participants was 32.49 years and 86% were males. Disordered gamblers, defined by PGSI (scored greater than 2), were randomized to receive brief advice with referral to treatment (intervention) versus referral to treatment only (control). The brief online advice lasted 10 min and included feedback regarding problem gambling, risk factors for development of severe gambling problems and strategies to reduce the risk of developing significant gambling-related problems. All participants received a list of gambling treatment resources which included referrals to helplines, self-help groups, and professional counselling in both Missouri and Illinois. The results highlight a high lifetime (86%) and 12-month prevalence (81%) of probable disordered gambling among the ex-offenders on probation or parole, although almost half (48%) with probable disordered gambling did not recognize their gambling to be problematic. Both groups had reductions in gambling frequency, positive attitudes towards gambling, and intensity of gambling (e.g., amount of money spent on gambling in the last 30 days). However, the difference in reduction between the two groups was not significant, suggesting that an examination of the intensity and acceptability of brief interventions is required to examine the efficacy of the effectiveness of online treatment for this population.
Incarcerated populations
327 male prisoners in a medium security federal prison (203 in the intervention and 124 in the control) were assessed before and after completion of a 20-week group psycho-educational programme (referred to as the Lifestyle Change Program: LCP) [7]. The control group were eligible to start the course but transferred to another prison before the programme began. The 20-week intervention focused on lifestyle issues; advanced criminal, drug and gambling lifestyle; and relapse prevention using cognitive behavioral approaches. The primary outcome measure was the total number of disciplinary reports; and secondary outcome included gambling related disciplinary reports. Those who participated in the programme had significantly fewer (29% reduction) disciplinary reports compared to the control group. However, due to the low incidence of reported gambling reports there was no evidence that participation in the programme was associated with a reduction in the number of gambling-related disciplinary reports. This was partly explained by the concern that gambling within prison is illegal and prisoners are therefore unlikely to provide self-report information of their gambling involvement. Participants in the intervention group were followed up for a significantly longer period of time than control participants (t (325) =2.06, p<0.05) and as such may have impacted on the results. Measurement and screening of gambling behavior in incarcerated populations requires careful thought to identify how best to record gambling behavior in this population.
Offenders with a criminal justice history in the community
231 randomly assigned pathological gamblers with a mean age of 44.9 years (SD 10.9) were assigned to one of three arms of a randomized trial that included referral to (i) Gambling Anonymous (GA), (ii) GA referral plus a cognitive behavioral therapy (CBT) workbook or (iii) GA referral and eight sessions of individual in person CBT [41]. Eligibility criteria for the trial included those who met DSM-IV criteria for pathological gambling, those who had gambled in the past 2 months, were 18 years or older, and could read at 5th grade level. The SOGS, ASI and ASI-G were used to assess the range and severity of problems related to gambling and were assessed at baseline, 1 month later, post treatment (2 months), and at 6- and 12- month follow ups. Secondary outcomes included a measure of the number of days gambled and the daily amount of money lost. The Service Utilization Form was used to evaluate user satisfaction with the interventions in the trial and psychiatric symptoms were measured using the Brief Symptom Inventory (BSI). Analyses were undertaken to compare participants with a self-reported history of gambling-related criminal activity in the past 12 months in a secondary analysis of this trial data [37].
Overall, gambling decreased among the majority of participants in all three treatment arms of the trial. Reductions in gambling with minimal interventions such as GA referral may be similar to results reporting in placebo arms of psychotherapy studies. The authors note that the workbook condition evidenced only marginal improvements, if any, relative to the GA referral alone. Decreases in psychosocial problems were dependent upon the treatment conditions with participants in individual CBT showing the greatest reductions overtime. Participants were significantly more satisfied with CBT treatments than with a GA referral alone. Existing treatment plans and programmes have the potential to become incorporated into existing programs to concurrently tackle physical and mental health problems alongside problem gambling (Table 2).
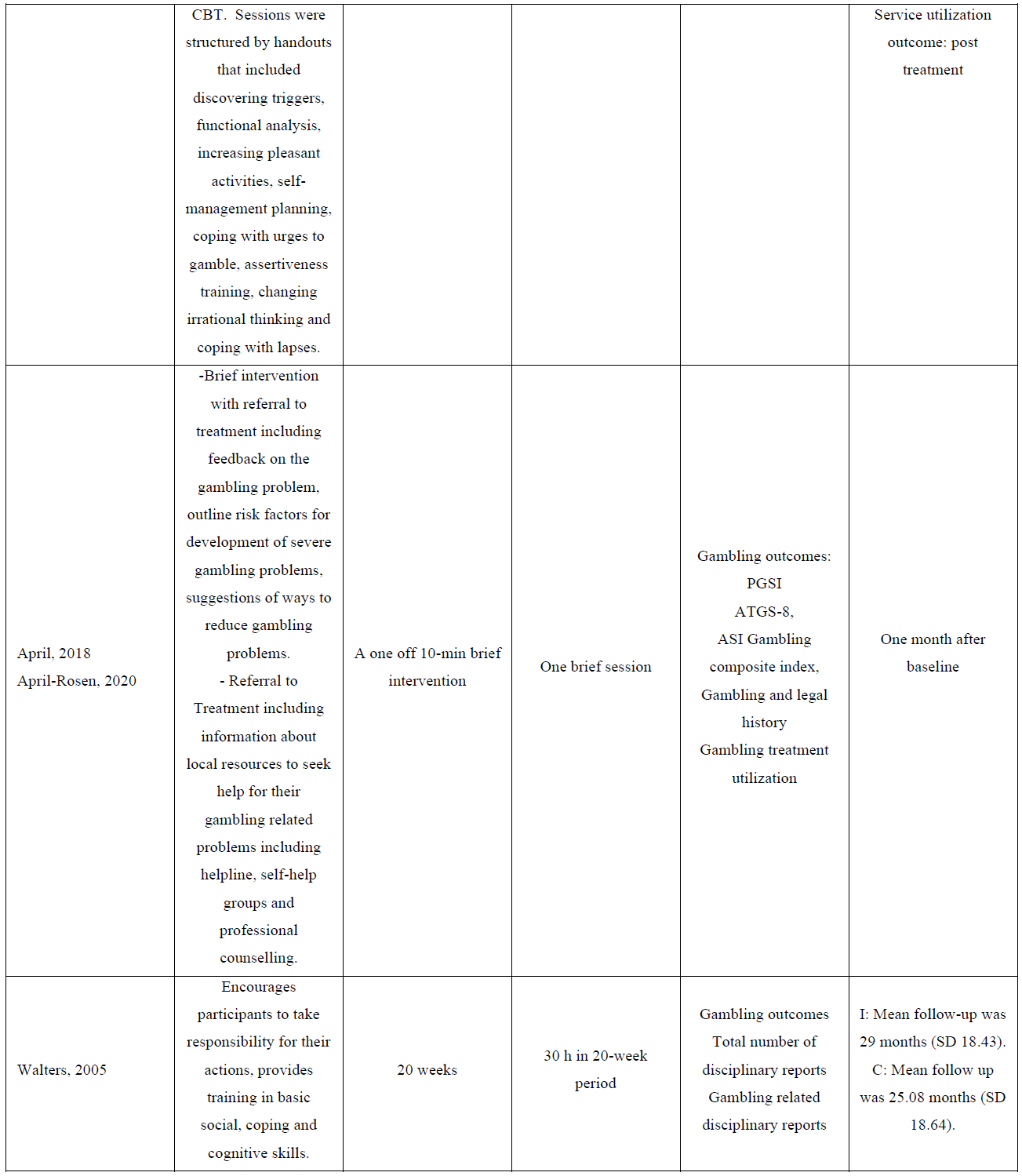
Risk of bias
Individual risk of bias domains (Figure 2) shows low risk of random sequence generation, one study was rated as ‘unclear’ in terms of allocation concealment. One study was at ‘high risk’ of attrition bias and another was rated as ‘unclear risk’. Both studies were rated ‘high risk’ of selective reporting.
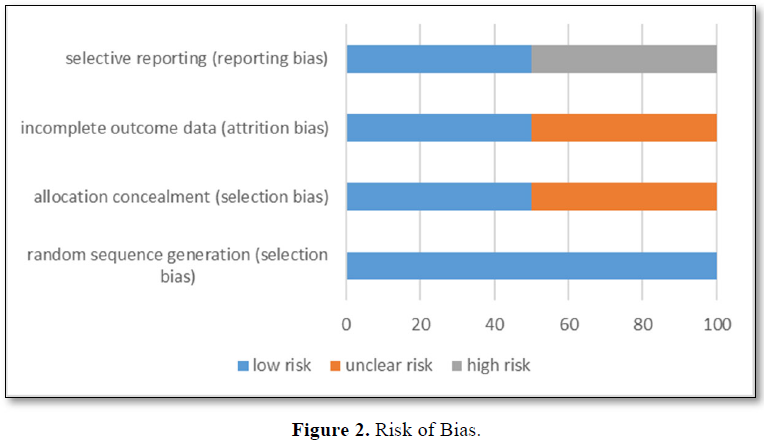
Using the JBI Critical Appraisal checklist, the single quasi-experimental study [7] was rated favorably in its clarity of ‘cause’ and ‘effect’ variables, with participation in the gambling intervention occurring before the outcome measures. Intervention and control groups showed they were similar in terms of age, offence history and follow-up, although not race. It was noted that only one post-test time point was used to collect outcome data. In addition, follow-up was complete and the outcomes measured reliably in the same way using appropriate statistical analyses.
DISCUSSION
Despite calls from the scientific community [25,42,43] the evidence to support the effective treatment of CJS involved people with problem gambling is sparse. Worldwide our systematic review identified only three studies evaluating the effectiveness of psychological interventions to reduce gambling behavior for people involved in the CJS. The three studies focused on populations under parole, those with a criminal history in the community and an incarcerated male population, all from the USA. Significant between group differences were not found across any of the studies, however gambling behavior was reduced across all treatment options except for the prison-based study that used a measure that wasn’t an acceptable reporting mechanism for the prison. None of the three studies reported on any of our secondary outcomes, although one study did report on the psychiatric symptoms of participants. The evidence about effectiveness of treatment for addressing the comorbidity of physical and mental health problems alongside gambling behavior is unknown. Methodological quality varied across the studies, but all presented some concerns in terms of risk of bias.
We therefore make a number of recommendations for future research:
CONTRIBUTORS
AP and AA were responsible for the overall design of the study. AP oversaw the day to day conduct of the study. RS was responsible for the development of search strategies. All authors conducted the pre-screening, secondary screening and data extraction of study information. All authors made substantial contributions to the interpretation of the data and drafting of the article.
DECLARATIONS OF INTEREST
All authors declare no competing interests.
ACKNOWLEDGEMENTS
This study was not funded. We would like to thank the support of the Centre for Reviews and Dissemination at the University of York for the advice provided on our search strategies.
FUNDING
None
REFERENCES
No Files Found
Share Your Publication :