-
Publish Your Research/Review Articles in our High Quality Journal for just USD $99*+Taxes( *T&C Apply)
Offer Ends On
Almón R, Angulo A, Escalona L and Brito A*
Corresponding Author: Brito A, Almón-Brito IPD Institute, Caracas, Venezuela.
Received: January 17, 2025 ; Revised: February 03, 2025 ; Accepted: February 06, 2025 ; Available Online: February 17, 2025
Citation: Almón R, Angulo A, Escalona L & Brito A. (2025) Comparison between Acellular Dermal Matrix and Connective Tissue Graft to Cover Multiple Gingival Recessions. Case Report. J Oral Health Dent Res, 5(1): 1-4.
Copyrights: ©2025 Almón R, Angulo A, Escalona L & Brito A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Views & Citations
Likes & Shares
Introduction: Subepithelial connective tissue graft (SCTG) is the standard treatment to cover exposed root surfaces. However, this technique has limitations such as the need for a donor site and the difficulty of the tissue obtaining procedure. The use of an acellular dermal matrix graft (ADMG) is proposed as an alternative treatment for the coverage of multiple gingival recessions.
Objective: To evaluate the effectiveness of ADMG for the coverage of multiple gingival recessions and compare its results with SCTG.
Methodology: A 61 years old female patient, with no systemic disease history, who initially came to the clinic for prosthetic treatment, was subjected to clinical examination. Bilateral gingival recessions RT2 in accordance to Cairo et al., (2011) were observed from the upper right canine to the upper left first molar. Split mouth surgical treatment is planned in combination with coronally advanced flap (CAF) + SCTG in the right upper quadrant and CAF+ADMG (OrACELL®) on the contralateral side. The length of the recession was measured before surgery and 45 days after surgery.
Results: The average percentage of root coverage was 75% on the side treated with SCTG and 92.5% on the surfaces treated with ADMG.
Conclusion: The results obtained in this case were satisfactory with both graft techniques with similar amount of root coverage, being slightly better in the gingival recessions treated with ADMG compared to the area treated with SCTG.
Keywords: Gingival recession, Subepithelial connective tissue graft, Acellular dermal matrix graft, Root coverage
INTRODUCTION
Gingival recession or soft tissue recession is defined as the displacement of the apical gingival margin to the cemento-enamel junction of a tooth or the platform of a dental implant [1,2]. According to the classification scheme of periodontal and peri-implant diseases 2018, gingival recession belongs to the category “Mucogingival deformities and conditions around the teeth” [3]. Gingival recessions are associated with factors such as the presence of dental biofilm, restorations at the gingival margin, anatomical characteristics such as muscular inserts near the gingival margin, reduced or absent band of attached gingiva, poor tooth alignment, reduced thickness of the alveolar bone and traumatic factors, therefore, the first step to achieve effective treatment is to identify the etiological factor associated with gingival recession [4].
Currently, the treatment of defects type recession is based on the use of periodontal plastic surgery procedures which include different surgical techniques aimed to correcting and preventing anatomical alterations, developmental, traumatic or plaque defects induced by diseases of the gum, alveolar mucosa or bone [2]. SCTG is the standard treatment to cover exposed root surfaces; however, this technique has limitations such as the need for a donor site and the difficulty in the process of obtaining tissue. The use of an ADMG is proposed as an alternative treatment for the coverage of multiple gingival recessions [5].
OrACELL® is an acellular dermal matrix of human origin that is used for the correction and reconstruction of soft tissues, guided bone regeneration and guided tissue regeneration. It is a highly biocompatible matrix that allows 97% of the DNA and cells to be eliminated without compromising the biological and biomechanical properties of the tissue, retaining all the necessary components of origin (growth factors, native collagen and elastin) that offers excellent integration in mouth.
The objective of this work is to evaluate the effectiveness of ADMG for coverage of multiple gingival recessions and compare its results with SCTG.
CASE PRESENTATION
The patient signed an informed consent form, thorough which she authorized the use of the data generated during the study for academic purposes in oral presentations and publications.
A 61 years old female patient, with no systemic disease history, who initially came to the clinic for prosthetic treatment, was subjected to clinical oral examination. During the evaluation, periodontitis stage III Grade A [6] and bilateral gingival recessions RT2 [7] of 4 mm were observed from the upper right canine to the upper left first molar. The exposed root surfaces showed severe wear caused by traumatic tooth brushing and tooth clenching. Split mouth surgical treatment is planned with CAF + SCTG in the right upper quadrant and CDC + ADMG (OrACELL®) on the contralateral side. The length of the recession was measured before surgical procedures and 45 days afterwards.
Prior to surgical treatment, the patient received periodontal treatment of scaling and root planning to eliminate local irritants and received instructions and training to improve her oral hygiene technique.
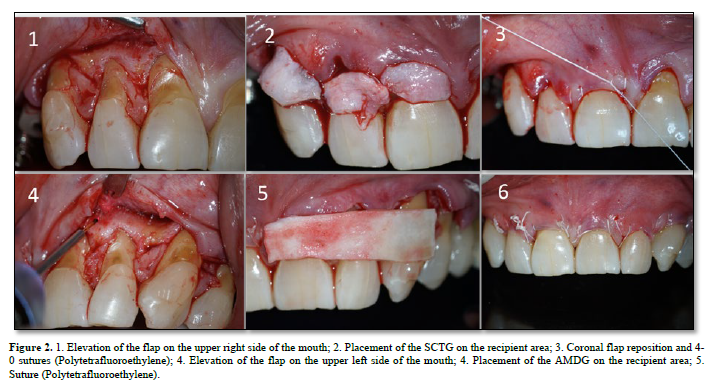
After sedation and local anesthesia, the exposed root surface was cleaned with manual and ultrasonic instruments. The recipient site was prepared doing an intrasulcular incision on the labial aspect of the affected teeth. Horizontal papilla-preserving incisions were made adjacent at the level of the cement-enamel junction. The mucoperiosteal flap was raised to the mucogingival junction, after this point, a partial-thickness flap was extended apically, releasing tension and favoring coronal positioning of the flap [8]. The epithelium of the adjacent papillae was de-epithelialized. The exposed root surfaces were smoothed with Gracey curettes (3/4) and rotatory instruments, followed by subsequent rinsing with sterile saline to obtain a surface free of organic debris and gently air dried. Donor tissue of appropriate size was taken from the posterior area of the palate, the tissue was cut out and prepared to be placed in the recipient area (teeth 11, 12 and 13). The graft was placed at the level of the cement-enamel junction to covers the recessions defects and was stabilized by using 4-0 non-absorbable suture (Polytetrafluoroethylene) and then sutured to the neighboring mucosa. The flap was then placed coronally with margins located in the coronal area of the cement-enamel junction. The flap was secured in position using horizontal suspensory sutures.
In the contralateral quadrant, an ADMG (OrACELL®) was placed following the manufacturer's instructions for hydration. The graft was trimmed and positioned from the cement-enamel junction and extended apically to cover the alveolar bone by at least 2 to 3 mm. The edges of the ADMG, basically the coronal and lateral sides were sutured to the lingual gingival tissue with 4-0 non-absorbable suture (Polytetrafluoroethylene). The flap was then placed coronally and sutured to cover the matrix (Figures 1 & 2).
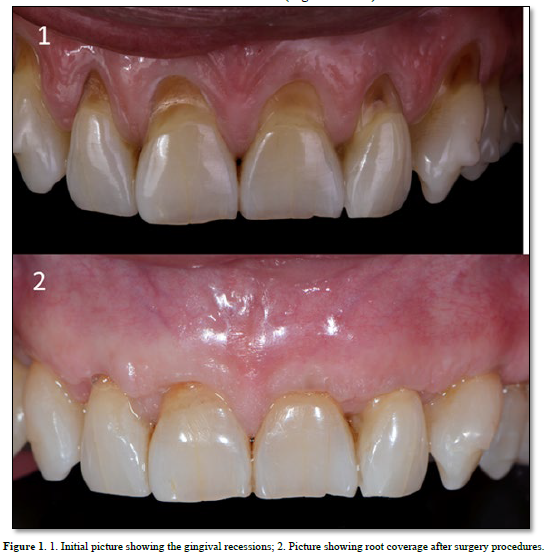
Oral clinical assessment was done seven days after surgery and then, one month and two months afterwards.
RESULTS
The initial length of the gingival recessions in the affected teeth was 4 mm.
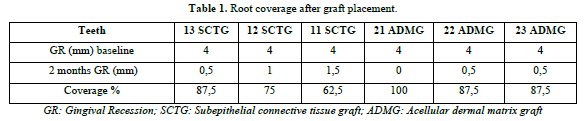
The results obtained in relation to the percentage of root coverage were the same on the canines (87,5%), however, on the upper central incisors the percentage of coverage was higher (100%) in the tooth where placed the AMDG.
The average percentage of root coverage after graft placement was 75% on the side treated with SCTG and 92.5% on the surfaces treated with ADMG (Table 1).
DISCUSSION
The SCTG combined with CAF or associated with another biomaterial can be used as root coverage procedures to treat localized or multiple recession-type defects. The available evidence indicates that in cases where both root coverage and an increase in the width of keratinized tissue are expected, the use of SCTG shows slightly better results than other techniques, however, this kind of graft has limited availability, especially when dealing with multiple gingival recessions. Furthermore, a second surgical bed is needed to take the donor tissue, which causes greater discomfort to the patient with a higher risk of bleeding due to damage to the branches of the palatine artery and the time of the surgical procedure is longer. In order to overcome this problems ADMG appear as the soft tissue substitute that may provide results most similar to those achieved with SCTG [9].
The objective of this case report was to compare the technique of SCTG + CDC versus ADMG + CAF for the coverage of multiple gingival recessions in the same patient. The results obtained in relation to the percentage of root coverage were the same on the canines (87,5%), however, on the upper central incisors the percentage of coverage was higher (100%) in the tooth where placed the AMDG.
In 2018, Chambrone [4] carried out a systematic review of periodontal plastic surgery procedures in order to find out which of them was most effective in reducing gingival recessions and found that there is no certainty about which intervention is the most effective and further research is needed. There is also weak evidence suggesting that ADMG appear as the soft tissue substitute that may provide results most similar to those achieved with SCTG.
Zhang [10] conducted a systematic review and meta-analysis to evaluate the efficacy and safety of connective tissue graft (CTG) versus ADMG for root coverage in patients with gingival recession and concluded that the use of ADMG may be superior to obtain clinical insertion gain, but with the CTG greater width of keratinized gingiva is obtained. They did not obtain significant differences between both procedures in terms of the percentage of root coverage, characteristics that in our case were more favorable in the teeth treated with ADMG.
Sood [9] conducted a comparative study between two groups of patients with gingival recessions. Their research results suggest that both techniques, a SCTG and ADMG with a CAF can produce an equivalent amount of aesthetic root coverage.
CONCLUSION
The results obtained in this case were satisfactory with both graft techniques with similar amount of root coverage, being slightly better in the gingival recessions treated with ADMG compared to the area treated with SCTG.
No Files Found
Share Your Publication :