-
Publish Your Research/Review Articles in our High Quality Journal for just USD $99*+Taxes( *T&C Apply)
Offer Ends On
Abu-Hussein Muhamad*, Abdulgani Azzaldeen, Alsaghee Maria, and Georges Chlorokostas
Corresponding Author: Abu-Hussein Muhamad, DDS, MSc D, MSc, M Dent Sci (Paed Dent), FICD, Center for Dentistry, Research and Aesthetics, Jatt /Israel.
Received: October 4, 2021 ; Revised: October 26, 2021 ; Accepted: November 29, 2021 ; Available Online: April 30, 2022
Citation: Muhamad AH, Azzaldeen A, Maria A & Chlorokostas G. (2022) Dental Implants in Children: An Update. J Oral Health Dent Res, 2(1): 1-9.
Copyrights: ©2022 Muhamad AH, Azzaldeen A, Maria A & Chlorokostas G. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Views & Citations
Likes & Shares
Abstract
Implants in a young patient have advantages such as improving bone quality, good osteointegration, wound healing and a healthy status of an individual but all these factors are overridden by a principle factor i.e., growth. Thus, the placement of an implant should be deferred until puberty or after the occurrence of growth spurt of the child. Patients and families should be educated about the fact that the placement of implants before the completion of growth could jeopardize the long-term esthetic outcome, since the remaining changes in the growing alveolar process will not be followed by the implant.
The aim of the present article is to review the skeleton and dental growth trend and its effect on the application of implant and present guidelines based on related articles and books for prescription and nonprescription of implant.
Keywords: Implants, Growth, Maxilla
INTRODUCTION
The replacement of teeth by implants is usually restricted to patients with completed craniofacial growth1 hence if the person in loss falls to be a child or an adolescent, it is definitely a nightmare for a Pediatric Dental Surgeon [1]. A replacement of the lost permanent tooth by implants is an obvious treatment modality of today in adult population but in children or adolescents, use of implants is yet a restrictional dilemma [2]. An implant is an artificial tooth root that is placed to support the replaced tooth or bridge, having being required in people who have lost their tooth/teeth due to trauma, dental caries, periodontal disease or some other reason [3]. However, in children who suffer from extended hypodontia, adontia, oligodontia or congenital syndromes as ectodermal dysplasia, the use of implants has become popular due to esthetic and functional reasons (Figure 1). This also reduces the potential psycho-social handicaps of the children [1,2,4].
Dental and skeleton growth is the greatest concern for placing implant in children and teenagers. The growth effect on implant position, implant impact, and its prostheses and on dental and skeleton growth will bring about some limitations in typical application of implant in growing patients [5,6]. High demands for using implant, due to more awareness of High demands for using implant, due to more awareness of parents of its positive psychological effects, as well as more inclination toward a more stable treatment and better physiological bone maintenance in congenital edentulous or traumatic areas, compared with removable prosthesis [7].
Researchers have been constantly working for a permanent or long-lasting solution for children suffering from tooth loss (Figure 2) [8]. This led to the thought that dental implants could be an option in growing children for transitional replacement which led to the clinical usage of narrow diameter non-Osseo integrating dental implants. Transitional implants are narrow diameter implants that were developed to support provisional fixed restorations during the phase of osseointegration of the definitive implants and are usually placed simultaneously with definitive implants [9-11].
Today many authors report successful placement of implants in children, however the long-term results on the stability, effect on alveolar bone growth and face etc. remains controversial [1-4]. Any surgical insult to the tissues in a growing phase can have a significant impact on the growth and development. In early childhood, increase in the width of the cranial base and the growth of the median suture influences the transverse growth of the maxilla. At puberty, the sutural growth is accelerated which if the first osntha lla three dimensions to be completed in a child during adolescence [1,2].
Even though there have been no problems reported in pediatric implants in the anterior maxillary region, an early implant placement in growing children can lead to diastema formation with the adjacent teeth as transverse growth occurs [3,4].
A multidisciplinary approach including the involvement of an orthodontist, pedodontist and a periodontist or an implantologist skilled in soft and hard tissue management around implants with a comprehensive treatment plan may be able to successfully place dental implants with a satisfactory long-term outcome in children suffering from congenital anodontia or multiple tooth loss [12-14]. However, implants might not be a reliable option for provisional single tooth replacement in growing children [1,3,14].
The aim of the present article is to review the skeleton and dental growth trend and its effect on the application of implant and present guidelines based on related articles and books for prescription and nonprescription of implant.
GROWTH
Growth in the maxilla and mandible does not happen uniformly in one plane. It is multidirectional, occurring in sagittal, vertical, and transverse planes. It does not happen at a fixed pace; slow periods of growth are followed by phases of accelerated growth called the growth spurts [1]. The teeth maintain their position in the arches by following this pace of growth through remodeling and drifting within the alveolar bone.
Functional forces are balanced by a stable interarch occlusal relationship, achieved gradually as transition from primary to permanent dentition occurs [3].
Maxillary Growth
Maxillary growth occurs as a result of sutural growth as well as by its passive displacement. During the primary dentition stage, passive displacement is the major contributor to its growth as the maxilla is carried downward and forward along the cranial base. After seven years of age, two thirds of maxillary growth occur by enlargement of the maxilla itself [1]. During early childhood, the transverse growth of the maxilla is influenced by the increasing width of the cranial base and growth at the median suture. This sutural growth accelerates at puberty and is the earliest of the three dimensions to be completed in adolescence [1].
Vertical growth of the maxilla occurs by sutural lowering of the maxilla and apposition on the tooth-borne surfaces of the maxillary alveolus. There is resorption on the nasal floor and deposition on the palatal and alveolar surfaces as the alveolus increase in height [2,3].
Mandibular Growth
The mandible being more closely associated with the cranial structures shows a differential growth as compared to the maxilla. This is more in the sagittal plane which is responsible for converting the more convex facial profile of the child to a straighter adult profile. The sagittal growth of the mandible is through endochondral growth in the condyle that extends the length but has no impact on the shape of the mandible as such [6].
The transverse growth in the mandible completes very early because of the closure of the symphysis in the 1st year of life, and only limited changes occur afterward through remodeling. Posteriorly, there is resorption of the bone lingually and deposition buccally that leads to remodeling. This pattern of bone growth may bring about lingual positioning of the implant in case it is placed early [15]. Increase in the mandibular length is limited posterior to the primary second molars to accommodate the permanent molars [3].
Growth in the vertical dimension occurs by the opposition at the dentoalveolar complex and rotation of the condyle that appears to displace the mandible downward and forward from the cranium. The vertical dimension is maintained through the dentoalveolar compensatory mechanism. This occurs when eruption proceeds normally, and there are no functional deviations [7].
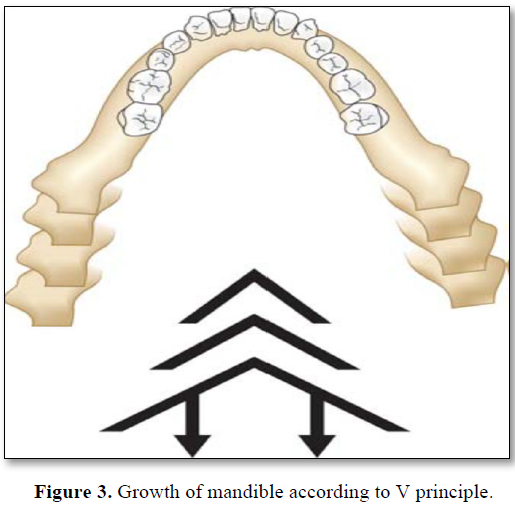
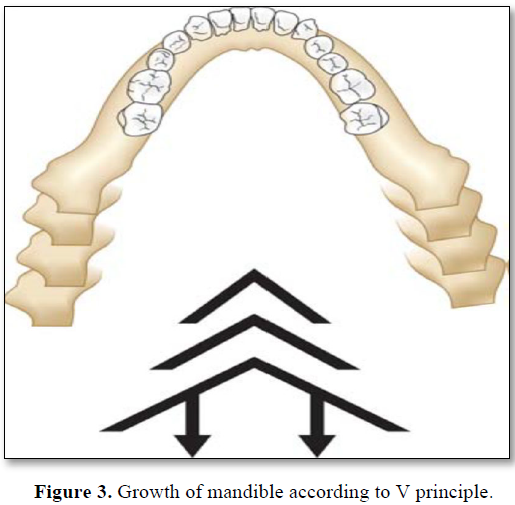
Endosseous implants (two in the maxilla and four in the mandible) were placed in a 3‑year‑old child with ectodermal dysplasia (ED). After a 5‑year follow‑up, implants placed in the anterior mandible moved with the mandible as growth occurred in the condyles and rami. The rotation of the mandible, which accompanies growth, did not cause a significant problem relative to the angulation of the implants and the prosthodontic occlusal plane (Figure 3). The maxillary implant however, was close to the nasal floor [2,3,5].
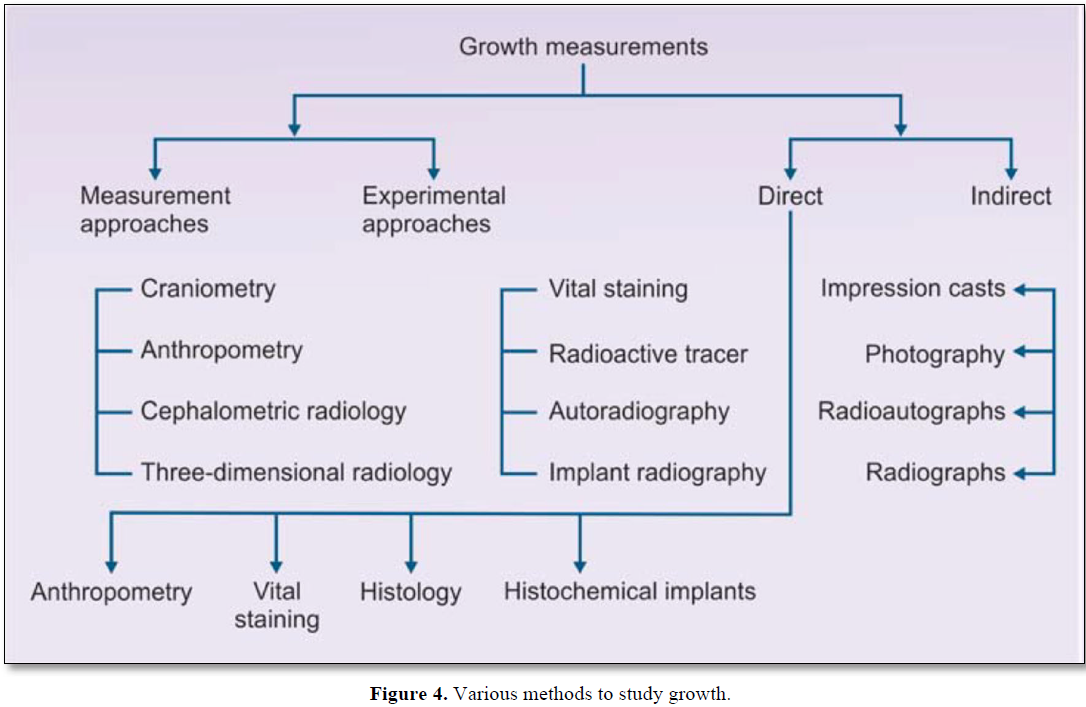
Montanari [16] reported a case of a child affected with ED accompanied with anodontia. At 2 years of age, conventional upper and lower prosthesis were made to allow for mastication and normal physiological development. At 11 years and 11 months, fabrication of lower implant supported dentures, and an upper conventional denture was indicated (Figure 4).
Mandibular growth in sagittal and transverse direction showed no adverse effects on implant position. After a 3‑year follow‑up, the implant supported overdenture was well accepted by the patient [2,6,16].
INDICATIONS FOR USE OF IMPLANTS IN ADOLESCENTS
CONTRA-INDICATIONS FOR THE USE OF DENTAL IMPLANTS
INDICATORS OF COMPLETION OF GROWTH
Chronological age is not sufficient to estimate growth cessation. Superimposing tracings of serial cephalometric radiographs taken at least 6 months apart (waiting until no growth change is seen over a period of 1 year) is probably the most reliable method, though it requires a lot of time and irradiation and may unnecessarily delay implant insertion [12].
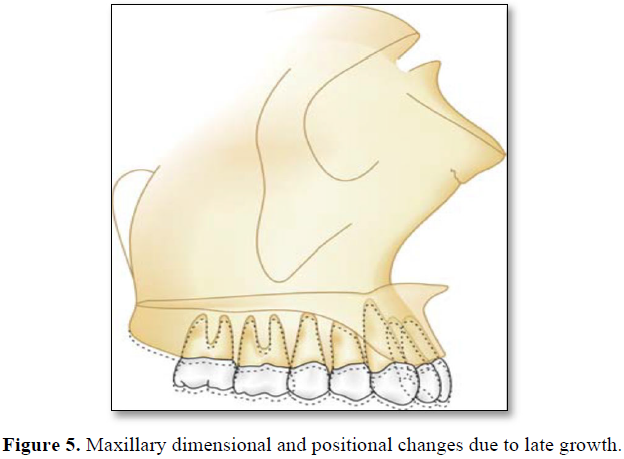
Skeletal growth status can be appraised fairly accurately by comparing a conventional radiograph of the hand and wrist against a standardized atlas of hand and the wrist bone development. Hand wrist radiograph indicators can be used to place a patient in the general area of the growth curve. Capping of the middle phalanges of the third finger (MP3cap) usually occurs after maximum growth velocity is completed and indicates a deceleration in the pubertal growth spurt. Once pubertal growth is completed, consideration of implant placement can begin (Figure 5). However, some risks still exist. When epiphysis of the radius fuses and forms a bony union with the diaphysis, adult level of skeletal growth has been attained and no further increase in statural height can be expected. This is the best and safest time to place a solitary implant [12].
CHOOSING A PROPER IMPLANT INSERTION AGE
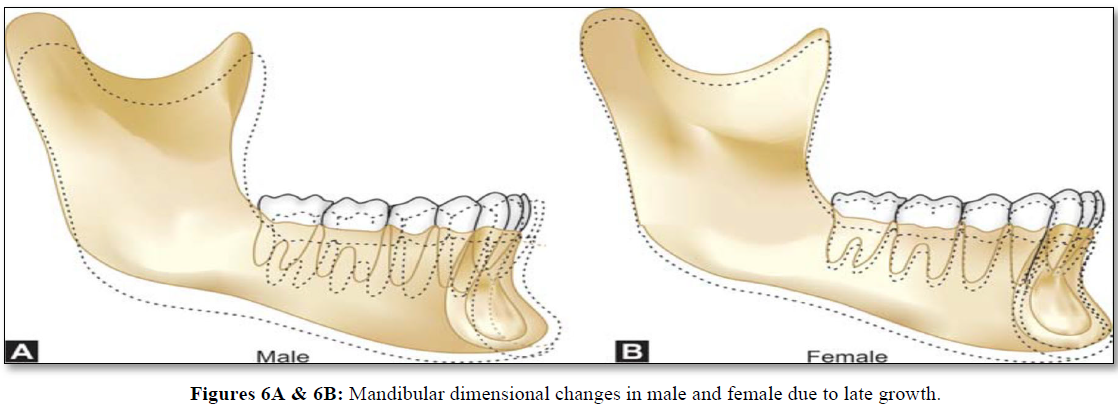
In cases of severe anodontia or oligodontia in the mandible, the possibility or necessity exists to place implants even before the pubertal growth spurt, since in this patient group few growth changes occur in the anterior region after the age of 5-6 years, especially because of the absence of teeth. For the maxilla, it is suggested to wait until after the growth spurt (Figure 6) [13].
During the consensus meeting in 1995 it was decided that implant placement especially in partially edentulous cases preferably should be postponed until the end of the craniofacial/skeletal growth [13].
Oesterle [17] observed that implants placed before the cessation of growth especially in the maxilla are unpredictable in their behavior and hence should be used with a great deal of caution. He suggested that implants placed during the pubertal period have a greater likelihood of success but still less than the post-pubertal or post-growth implant.
Cronin [18] observed that if implants are placed during active growth, they may be displaced or malpositioned by continued growth and may require removal and replacement. Implants placed after age 15 for girls and age 18 for boys have the most predictable prognosis. Implants placed before these ages may not be permanent and may have to be re-implanted (Figure 7).
RECOMMENDATIONS BY AREA FOR PLACING AN IMPLANT
Anterior maxilla
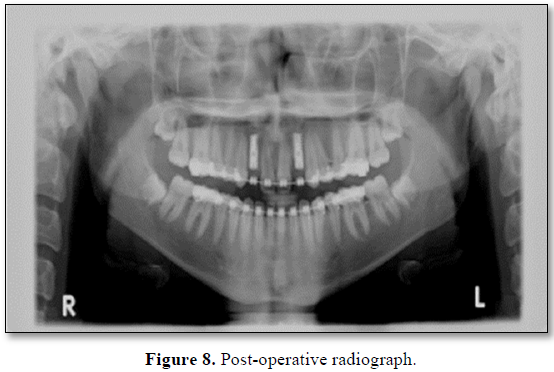
It is the riskiest site for early implantation due to the unpredictability of growth in the area, especially in the presence of natural teeth (Figure 8). Premature implant placement can necessitate a repeated lengthening of the transgingival or transmucosal part of the implant, resulting in a poor implant - prosthesis ratio and adverse load magnification. It is advised to delay implant insertion until after skeletal growth is completed [1,2,17].

An early inserted implant can become submerged occlusally and exposed apically because of resorption of bone in the maxillary sinus/floor of the nose. It is recommended to delay an implant placement until after cessation of growth [1,2].
Anterior mandible
This site seems to hold the greatest potential for early use of an implant supported prosthesis. However, use of early implants in combination with teeth is not advisable due to the significant compensatory change in the dentition in this area during growth [1,2,19].
Posterior mandible
It is recommended to delay implant placement until skeletal growth is completed as progressive infraocclusion of the implant and harm to adjacent teeth preclude the early placement of implant in this site [1,2,17,19].
DISCUSSION
Successful implant treatment in children has been achieved by several clinicians when they incorporated a multidisciplinary approach in their treatment plan. The Child patient is seen by the pediatric dentist at a very small age and remains under his care for a long period giving sufficient time for appropriate treatment planning.
Important factors to be considered when treating a child with missing tooth, apart from growth, are dentition present, residual space between the teeth present in the arch, amount of alveolar bone, and the timing of implant placement [1,3]. Preservation of primary teeth till their root resorption, prevention of caries or endodontic treatment to prevent any periapical pathology and subsequent bone loss is important for later implant placement. It prevents the loss of arch length and maintains the alveolar bone height. The pediatric dentist should be capable of managing the primary dentition to create a healthy oral cavity for future [17,19].
Ryda [20] suggested that all the clinical judgment and treatment for children should be performed according to the United Nations Convention on the Rights of the Child.
Child's development physically as well as psychologically should be respected while planning the treatment. [20]. Children of age six years and above can undergo implant placement in mandibular anterior regions in cases of anodontia whereas children of around 3 years of age should be treated only by removable prosthesis as recommended by National foundation for Ectodermal Dysplasia USA [20].
According to Kraut [21], 15 years of age in girls and 17 years of age of boys should be waited for implant placement at maxillary anterior & posterior regions. Mandibular anterior region is the most ideal area for the Osseo integrated implants placement prior to the growth. During the first two years of life, the suture in the symphysis region becomes closed. Implant supported prosthesis in mandibular anterior region should be re-designable in order to allow for a 5-6- mm increase in dental height as well as anterio-posterior growth [18].
Montanari [16] advocated a dental multidisciplinary team that includes a pediatric dentist, an orthodontist, a prosthodontist and an oral and maxillofacial surgeon for a successful outcome in implant placement in children. They carried out the oral rehabilitation in a child with hypohidrotic ED with an implant supported overdenture.
Conventional dentures were made for the child at the age of 2 years. At the age of 11 years and 11 months, an upper conventional denture and a lower implant supported
overdenture was made. Two tapered screw endosseus implants were placed in the anterior aspect of the mandibular jaw. After a healing period of 2 months, the implants were exposed, and two ball‑attachments were connected to the implants to avoid a rigid connection [16].
This was done to allow normal mandibular growth and to reduce interference with the patient’s growth. The prosthesis was connected with implants using the two ball‑attachments. After 3 years of follow‑up, the mandibular implant supported overdenture was well accepted from the patient who reported excellent masticatory and esthetic improvements [16].
Smith [22] reported the possibility of implant positioning in children aged even
According to some studies, implant positioning should be avoided in children aged <16-18; otherwise, the tooth will erupt with infraocclusion shape in proportion to the alveolar bone and will remain at the opposite position. According to Bergendal [23] only in full aplasia case, like what is seen in ectodermal dysplasia, early implant positioning is applicable, as well [23,24]. However, by emphasizing on no affiliation with any implant manufacturer, Erosy despite vertical and transverse growth of adjacent bone to the implant, evaluated the developmental difference of these two areas at correctable and improvable level and declared that early implant placement could affect the maintenance and growth of bone [24]. Evaluating the effect of implant on factors including manner of dental and skeletal development, place and extent of edentulous, edentulous reasons (hereditary, along with an especial syndrome, trauma, tumor), range of remaining growth, application as an orthodontic support and the material and time of usage could affect implant positioning [23,24].
Ledermann [25] used the titanium (Ti) implant system in their patients. The implant features a highly polished neck with the dimension of a natural tooth, and a step screw implant shape analogous to a natural tooth root. implants were placed in 34 patients, aged 9-18 years through a 7year period. Their follow up has been associated with a success rate of 90%. Guided tissue regeneration procedures using Gortex or Vicryl membrane were used in two patients showing bony dehiscence after the implant was completely inserted. They stated that when a root form implant is placed into an alveolus immediately after tooth loss, the degree of resorption can be minimized even when narrow bone dimension results in a dehiscence after implantation [25].
Valle [26] successfully treated a case of hypodontia in a child by a multidisciplinary treatment approach. The pediatric dentist maintained the primary second molars till the child was 17‑year‑old and then combined with orthodontic treatment to allow for space sufficient for the placement of endosseous implants. Later when the primary teeth were extracted, external hex implants with a 4.1 mm rectangular platform were placed with immediate load [26].
Performed a retrospective study on 328 adolescents with congenital anodontia of permanent maxillary anterior teeth between the years 1990 and 2005 [27]. A total of 276 implant sites were restored in 255 patients. Orthodontic treatment was performed in all the cases. The final root position and angulation of the permanent teeth in the premaxillary region were established. Stabilization of the occlusal relationship between the arches was carried out before implant placement. Bone grafting was done wherever needed to improve the hard tissue topography and ensure a harmonious crestal ridge contour for a better esthetic outcome. Orthodontic retainers were given to all the patients during the initial bone healing phase of the implant. There were no implant failures during the 15 years of this report after the final prosthesis delivery [27].
Placed the implants at a distance of least 1.5 mm from the adjacent teeth. Implant length range was 12-16 mm and the body diameter varied from 3.5 mm to 4.0 mm. This was based on the mesiodistal dimensions of the missing tooth and the buccolingual dimensions of the bone. All implant bodies were of a two-piece screw design in which surface treatment was done with a resorbable blast media or hydroxyapatite (Ha). All implants were left unloaded during the initial bone healing process [28]. Johansson [29] placed a single tooth implant in a boy who was 12.3 years old. He followed the case up for 4.5 yrs. It was observed that the fixtures did not move together with the adjacent teeth and the maxillary growth went on uninterrupted causing submergence of the implant at sight [27]. Conducted a prospective clinical trial. The effect of endosseous dental implants on the mandible of children with ED was studied in twenty-three adolescents (12-17 years) and 12 preadolescents (7-11 years). 225 implants were placed in all. Twenty-two implants failed with a success rate of 91.3% (preadolescent group 88% and adolescent group 90%). They concluded that Osseo integrated implants in children with ED seem to be a feasible treatment [27], found that mini-implant placement in adolescent patients did not require osseointegration for immediate loading and showed long-term potential stability when integrated under functional biting forces [31]. Conducted a study in a 4-year-old ED patient. Mandibular endosseous implants were paced. Follow-up of 6.3 years was done. After loading, vertical growth pattern changed to low angle due to lack of alveolar growth in time. Correction by changing the vertical heights of the abutment and prosthesis was done. They concluded that early implant placement and fixed prosthesis could be a good treatment option for ED patient.
Heij [32] osseointegration of implants in a growing child is not in par with spontaneous and continuous eruption of natural dentition. Such an implant has a tendency to disturb normal development of the jaw bones.
Development of the jaw in the immediate vicinity of implants is slowed down, leading to unesthetic and nonfunctional situation. The result is loss of occlusal contact and periodontal complications such as angular bony defects around the adjacent tooth [6]. Delaying implant placement may sometimes render treatment options impossible as resorption following tooth loss may lead to insufficient volume of bone than needed for implant placement. However, if this resorption can be prevented by immediate implant placement remains a question unanswered [5,6].
Pigno [33] found that immediate implant placement was beneficial to preserve alveolar bone and those implants which were placed at an age of 15 years in girls and 18 years in boys showed a good prognosis.
Prachar and Vaneek [34] conducted a 5-year study on the use of cylindrical or screw implants in 135 adolescent patients aged 15-19 years. 191 implants were placed. The clinical success rate was accessed by means of selected criteria, i.e., patient’s sex, the type of implant, the cause of tooth defect, and the type of prosthetic reconstruction supported by implant. Regardless of the criterion used, the rate of success was >96% over the 5 years of study of tooth defect, and the type of prosthetic reconstruction supported by implant.
Iseri and Solow [35] revealed that the eruption of upper jaw teeth might have a strong effect on implant treatment, such that the average annual eruption rate during development ages is 1.2-1.5 mm and the compensation of such alterations using the implant asks for 9-10 tough years in girls and is impossible in boys [36]. Any changes in palate height were also assessed by some Scientists as they calculated the distance between occlusal section and palate section about 2.5-6 mm. This amount includes the increase of alveolar height and vertical height of permanent detention [21]. The remarkable growth of bone height, especially at posterior palate, might cause the implant to be buried more than one centimeter at posterior maxilla and even the apical level to be appeared at the base of nasal cavity [35].
McDonald [15] suggested that implant positioning in anterior maxilla, with the most single hereditary and acquired edentulous, should be postponed due to existence of various joints and bone stability delay until the completed growth before puberty.
According to some studies, implant positioning should be avoided in children aged <16-18; otherwise, the tooth will erupt with infraocclusion shape in proportion to the alveolar bone and will remain at the opposite position [3,4,27].
Most studies alerted the early application of implant in growing children [38,39] and most dentists prefer to perform the implant treatment after the sexual maturity [2].
The timing of implant placement in growing patients was discussed at a Scandinavian Consensus Conference in Snooping, Sweden [32], where there was a general agreement that implant placement should be postponed until skeletal growth is completed or nearly completed in normal adolescents. In the individual with Oligodontia or anodontia, however, earlier intervention could be indicated, especially in the mandible (Figure 9) [5,8-11].

CONCLUSION
Implants in a young patient have advantages such as improving bone quality, good osteointegration, wound healing and a healthy status of an individual but all these factors are overridden by a principle factor i.e., growth. Thus, the placement of an implant should be deferred until puberty or after the occurrence of growth spurt of the child. Patients and families should be educated about the fact that the placement of implants before the completion of growth could jeopardize the long-term esthetic outcome, since the remaining changes in the growing alveolar process will not be followed by the implant.
Various studies have suggested that use of implant, due to developmental changes of jaws and teeth in children, should be performed with high precision and systematic evaluation and, if possible, be postponed up to the age 15 for girls and 18 for boys, and be within a long-term process [40]. On the other hand, the evaluation of some factors, including causes of anodontia, patient’s sex, range of skeletal growth, prosthesis design, the range and quality of residual bone ridge, keeping hygiene and satisfying parents and patients’ demands should be taken into consideration for final decision-making on implant positioning.
REFERENCES
No Files Found
Share Your Publication :