-
Publish Your Research/Review Articles in our High Quality Journal for just USD $99*+Taxes( *T&C Apply)
Offer Ends On
Duaa Aboalsamh*
Corresponding Author: Duaa Aboalsamh, Dental Department, Prince Sultan Military Medical City, Riyadh, KSA, Saudi Arabia
Received: January 22, 2021 ; Revised: February 03, 2021 ; Accepted: February 05, 2021 ; Available Online: December 28, 2021
Citation: Aboalsamh D. (2021) Non-Surgical Endodontic Treatment of Extra-Oral Cutaneous Sinus Tract: Case Reports. J Oral Health Dent Res, 1(1): 1-4.
Copyrights: ©2021 Aboalsamh D. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Views & Citations
Likes & Shares
Sinus tract or fistula are mainly a common manifestation of pulpal necrosis that usually requires conventional endodontic treatment in order to heal. They are identified intraorally and in rare cases manifest extra-orally. Such conditions may be misdiagnosed and confused with other non-pulpal pathologies. Thus, the differential diagnosis of this clinical dilemma is important in providing correct clinical care and preventing unnecessary and non-effective treatment and healing failure.
Facial fistulas of endodontic origin, despite sparse, should be considered as an option in the differential diagnosis procedure.
Once the correct diagnosis is made, definitive treatment through root canal treatment or tooth extraction will eliminate the source of infection and lead to healing.
In this case report an extraoral sinus tract was initially misdiagnosed by a physician as a non-odontogenic lesion. However, after conventional root canal treatment complete healing was observed.
Keywords: Sinus tract, Endodontic treatment, Extra-oral cutaneous fistula, Odontogenic fistula
CASE REPORT
A healthy 45-year-old female was referred to our endodontic clinic to treat lower right first molar tooth # 46 with endodontic lesion.
The patient had no complaints of dental pain or other dental symptoms.
During the initial extraoral examination, a red discolored lesion was noted on the right check (Figure 1). The patient recalled that it started 16 months ago, as a small skin lesion associated with a white spontaneous drainage.
A physician started treating this lesion as skin infection and the patient was given an appointment for surgical removal of the sinus tract extra-orally. she was started on systemic antibiotic and according to the patient, the lesion and associated sinus tract were only transient subsided, but never completely healed.
Clinical examination revealed tooth # 46 with big composite resin felling. Tooth was not sensitive to percussion and palpation and gave negative response to cold test.
Radiographic examination of tooth # 46 reveled diffuse periapical radiolucency associated with the mesial root (Figure 2).
The clinical diagnosis was established as chronic periapical abscess with an extraoral sinus tract.
After local anesthesia inferior alveolar nerve block using 2% solution of lignocaine hydrochloride containing 1:80000 adrenaline (Lignox 2% A, Warren, Indoco) and rubber dam placement on tooth # 46, root canal treatment was initiated with pulp chamber access and chemo mechanical preparation.
The root canal systems were cleaned and shaped using nickel titanium rotary files (easy Race, Sybron Endo, Orange, California, USA) up to size 35, 0.04 tapered in crown down manners and irrigated with 2.25 % Sodium Hydroxide solution.
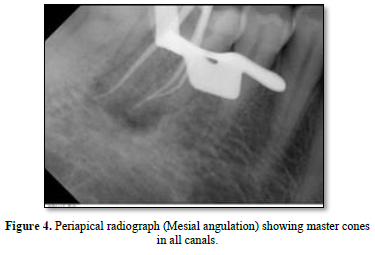
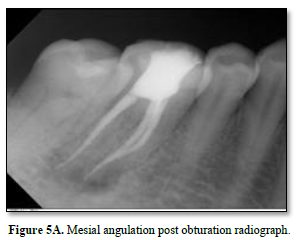
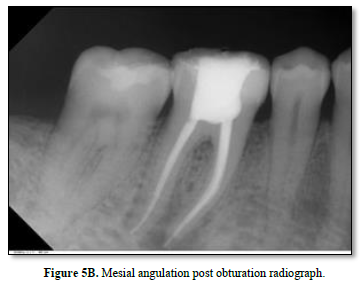
Canals were dried and Calcium hydroxide paste was placed in all canals as an intracanal medicament and the tooth sealed with IRM (caulk/DENTSPLY Milford, Delaware, USA). After one month from the initial appointment, the extraoral lesion showed remarkable healing (Figure 3). Master Gutta Percha cones (DENTSPLY) were placed in the canals and a radiograph taken (Figure 4). The root canals were then obturated with Gutta-Percha points and root canal sealer AH-plus, Dentsply- mellefer, Ballaigues (VD), Switzerland, using the lateral condensation technique. The occlusal access opening was sealed with temporary felling material and post-obturation radiographs were taken to evaluate the quality of obturation (Figure 5 A and B) Patient was then referred for permanent restoration and crown.
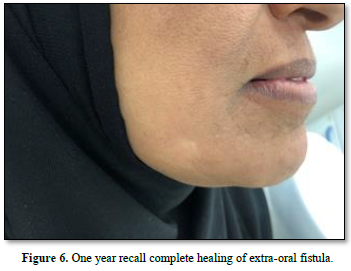
After one-year recall, complete healing of the extraoral fistula was observed clinically (Figure 6) and post-operative radiograph showed complete healing of the periapical radiolucency (Figure 7).



DISCUSSION
When a draining lesion is observed on the facial skin, an endodontic origin should always be considered in the differential diagnosis including suppurative apical periodontitis, osteomyelitis, salivary gland fistula, infected cyst, and deep mycotic infection [1].
A cutaneous fistula of dental origin is a pathway that begins at the apex of an infected tooth or of the infected region of the jaw through the alveolar bone and drains infected materials (pus) through the skin [2,3]. For proper treatment of this situation, an accurate diagnosis is essential.
After extraoral, intraoral and radiographic examination if the lesion is from dental origin the main approach should be to cut off communication between the infected area and the skin (to eliminate the source of infection) [4-6]. Intraorally this can be done by nonsurgical conservative endodontic therapy [7]. In certain cases, apical resection or extraction with curettage and surgical removal of the sinus tract extra orally may be necessary [8].

Diagnosis is challenging for many reasons; this can be due to the fact that these lesions do not always arise in close proximity to the underlying dental infection and only about half of the patients ever mention having had a tooth ache [9,10].
Palpation of the involved area often reveals a cord like track in the area of suspected tooth. Intraoral examination may reveal carious or discolored teeth. The involved teeth may respond negatively to pulp vitality test [10-14].
As suggested in the literature, conventional endodontic therapy is the treatment of choice of such lesions and should be attempted first [15].
If correctly diagnosed and treated, the sinus tract is expected to disappear within 7 to 14 days [16]. In this case healing was noted following the initial treatment.
Calcium hydroxide paste was used as an intracanal medicament for its rapid and successful treatment of sinus tracts associated with necrotic teeth [6,10,12].
Usually there is no need for systemic antibiotic as the lesion is localized. It has been observed that systemic antibiotic therapy will result only in a temporary reduction of the drainage and pseudo healing [9,12,17,18].
CONCLUSION
Dental etiology should be considered as part of any orofacial skin lesion. In this case report, the elimination of infection through nonsurgical root canal treatment led to the resolution of the sinus tract and promoted periapical healing of the involved tooth. Communication between the dentist and the physician is essential to provide timely recognition and treatment of such cases.
No Files Found
Share Your Publication :