-
Publish Your Research/Review Articles in our High Quality Journal for just USD $99*+Taxes( *T&C Apply)
Offer Ends On
Ayaz Ali*, Jhoset Molinares Hernandez, Anwar Ali, Kinjal Shah, Muzamil Khan, Sidra Kamal, Meibrahim, Ruchira Clementina, Mubashir Ali Aftab and Afaq Ahmad
Corresponding Author: Ayaz Ali, Internal Medicine, Khyber Medical College, Peshawar, Pakistan.
Received: July 17, 2024 ; Revised: July 28, 2024 ; Accepted: July 31, 2024 ; Available Online: August 14, 2024
Citation: Ali A, Hernandez JM, Ali A, Shah K, Khan M, et al. (2024) Comparative Analysis of Pulmonary Health among Traditional Smokers, Non-Smokers and E-cigarette Users: A Cross-sectional Study. J Oral Health Dent Res, 4(2): 1-9.
Copyrights: ©2024 Ali A, Hernandez JM, Ali A, Shah K, Khan M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Views & Citations
Likes & Shares
Background: Respiratory diseases represent a major global health challenge, with smoking being a primary risk factor. The emergence of electronic cigarettes (e-cigarettes) as an alternative nicotine delivery system has sparked concerns about their potential impact on pulmonary health. Understanding these risks is crucial for effective public health policies and interventions.
Electronic cigarettes (e-cigarettes) are battery-operated devices that heat a liquid (e-liquid) to generate an aerosol, which users inhale. This aerosol typically contains nicotine, flavorings, and other chemicals. While marketed as safer alternatives to traditional cigarettes, the long-term health effects of e-cigarettes remain uncertain, particularly concerning respiratory health. Studies have suggested links between e-cigarette use and respiratory symptoms, but comprehensive research comparing their effects with traditional smoking is limited.
Methods: Conducted at the University of Peshawar, Pakistan, this study employed a cross-sectional design to analyze data from adults aged 18 years and older. Participants were categorized into three groups based on their smoking habits: e-cigarette users, traditional smokers, and non-smokers. Sampling techniques included random and snowball sampling methods. Data collection involved structured questionnaires to assess smoking behaviors and respiratory symptoms, complemented by clinical assessments such as pulmonary function tests.
Results: Among the study's participants (mean age 30.67 years; 80% male), a significant proportion reported using e-cigarettes (53.3%), and traditional cigarettes (26.7%) or were non-smokers (20%). Analysis revealed a high prevalence of respiratory symptoms among e-cigarette users, including frequent coughing (100%), shortness of breath (100%), and diagnoses of obstructive lung diseases (86.1%). Comparative analyses demonstrated statistically significant differences in respiratory health outcomes across the three smoking groups (p < 0.001), highlighting distinct risks associated with each category.
Discussion: The findings underscore the substantial respiratory risks associated with emerging e-cigarette technologies, comparable in magnitude to those seen with traditional smoking. Socioeconomic factors appeared to influence smoking behaviors, suggesting targeted interventions are necessary to address these disparities effectively. This study contributes valuable insights into the complex interplay between e-cigarette use, respiratory health, and public health policy, calling for continued research and evidence-based regulatory measures.
Conclusion: In conclusion, this cross-sectional study provides compelling evidence of significant respiratory risks associated with emerging e-cigarette technologies. The findings emphasize the urgent need for further research to elucidate long-term health effects and inform comprehensive public health strategies aimed at reducing the prevalence and impact of e-cigarette use on pulmonary health.
Keywords: E-cigarettes, Pulmonary health, Respiratory symptoms, Cross-sectional study, University of Peshawar
INTRODUCTION
Respiratory diseases are the major cause of morbidity and mortality in the United States [1]. Smoking is a major cause [2] E-cigarettes (Electronic) produce an aerosol of nicotine by heating a solution containing nicotine, propylene glycol, glycerin, and flavorings [3]. Some pulmonary toxicants, such as propylene glycol, diacetyl (butter flavor), cinnamaldehyde (cinnamon), benzaldehyde (cherry), and metals, are found in e-cigarette aerosol in higher amounts than in combusted cigarettes [4].
E-cigarettes have been pushed for smoking cessation even though, as of November 2020, no e-cigarette has been certified as a smoking cessation therapy by the FDA Centre for Drug Evaluation and Research [5]. In addition to combustible tobacco smoking, the use of e-cigarettes increases the chance of developing respiratory disease. Dual use, the most common use pattern, is riskier than using any product alone [6]. Current e-cigarette usage appears to be an independent risk factor for respiratory disease, in addition to all combustible tobacco use. Moving from combustible tobacco, including cigarettes, to e-cigarettes may theoretically lessen the chance of acquiring respiratory disease [6]. After ten years of experience with electronic cigarettes (e-cigarettes), it is established that their active usage is connected with immediate negative health effects [7].
E-cigarette use and household SHA exposure were independently linked with asthma symptoms in teenagers. Thus, such data show that e-cigarette usage and passive exposure to their aerosols have a deleterious influence on respiratory health among adolescents [8].
Although the long-term effects of regular e-cigarette use are unknown, multiple research, including early longitudinal data, indicate that e-cigarette usage is associated with an increased risk of respiratory disease, regardless of contemporaneous traditional cigarette consumption. Improved understanding and recognition of harm will contribute to the basis of subsequent studies evaluating the influence of e-cigarettes on chronic respiratory disease, as well as future prevention education [9].
In support of a putative incidental link between hypoxia and depression, discovered that three markers of chronic hypoxia (COPD, smoking, and high altitude) were related to suicide and that this risk was more prominent among patients who had two or three risk factors [10].
Cohort studies have also found that cigarette smokers have a higher risk of developing asthma. To further the relationship between tobacco exposure and asthma, secondhand exposure to smoking should be considered [11].
Airway irritation, mucus hyper secretion, and an inflammatory response, including systemic changes, have all been documented following e-cigarette use, resulting in an increase in respiratory symptoms as well as changes in respiratory function and host defense mechanisms [12]. According to the survey results, even after controlling for potential confounders, EC use increased the likelihood of being diagnosed with asthma when compared to the reference population. EC usage was also associated with an increase in asthma severity, as measured by days missed from school due to symptoms [13]. In general, ECs have been utilized as smoking cessation aids or as substitutes for traditional cigarettes (CCs) [14]. Some research imply that the EC contributes to the reduction or cessation of cigarette smoking [15], while others criticize it as a dangerous substance in its own right [16].
Asthmatic individuals smoke at about the same rate as the general population, with 26% being active smokers [17]. Asthma severity, quality of life, unplanned healthcare visits, and hospitalization are all linked to smoking [18,19].
OBJECTIVES
Determine the prevalence of respiratory symptoms and conditions among users of emerging e-cigarette technologies.
Compare pulmonary function between users of emerging e-cigarette technologies, traditional cigarette smokers, and non-smokers.
Assess the types of emerging e-cigarette technologies being used and their characteristics.
METHODS
Study setting
This study was conducted at the University of Peshawar, located in Peshawar, Khyber Pakhtunkhwa province, Pakistan.
The University of Peshawar was chosen due to its diverse population, which will provide a representative sample for the study.
Study Design
This study is a cross-sectional analysis designed to investigate the long-term pulmonary health effects associated with the use of emerging e-cigarette technologies.
Study Population
The study will include participants who are 18 years of age or older. Participants will be divided into three groups: users of emerging e-cigarette technologies, traditional cigarette smokers, and non-smokers who are exposed to environmental tobacco smoke.
Inclusion Criteria
Participants must be 18 years of age or older, users of emerging e-cigarette technologies, traditional cigarette smokers, or non-smokers, and willing to provide informed consent.
Exclusion Criteria
Participants who are under the age of 18, have a history of chronic respiratory diseases unrelated to smoking or e-cigarette use or are unable or unwilling to provide informed consent will be excluded from the study.
Sampling Technique
A combination of random sampling and snowball sampling was employed to recruit participants. Initial participants were selected randomly from the university population. These participants were referred to additional subjects who met the inclusion criteria, helping to expand the sample size and diversity.
Sample Size
To determine the sample size, we utilized the formula:
Where SS is the Sample Size, Z is 1.96
(reflecting the 95% confidence level), P is the Expected Prevalence or Proportion (approximately 53% from previous studies), and D is the margin of error (0.05). By inputting these values into the formula, we calculated an approximate sample size of participants which is approximately 384.
Data Collection
Data was collected through a combination of self-administered questionnaires and clinical assessments:
Questionnaires: Participants completed a detailed questionnaire covering demographics, smoking history, use of e-cigarette technologies, and respiratory symptoms. The questionnaire also gathered information on the types and characteristics of e-cigarette devices used.
Clinical Assessments: Pulmonary function tests (PFTs) were conducted to measure lung function parameters, including Forced Vital Capacity (FVC) and Forced Expiratory Volume in one second (FEV1). These tests were administered by trained healthcare professionals using standardized equipment and protocols.
Data Analysis
The analysis was done using SPSS software version 20 and the p-value was considered significant which was equal to or below 0.05. Descriptive statistics were used to summarize the prevalence of respiratory symptoms and conditions among the different groups. Comparative analyses, such as chi-square tests, were performed to compare pulmonary function between users of emerging e-cigarette technologies, traditional cigarette smokers, and non-smokers.
Ethical Considerations
The study was conducted in accordance with the ethical principles outlined in the Declaration of the Institutional Review Board of Khyber Medical College. Informed consent was obtained from all participants prior to their inclusion in the study. The study protocol was reviewed and approved by the Institutional Review Board (IRB) of the Khyber Medical College and the University of Peshawar.
Expected Outcomes
The study aims to provide insights into the prevalence and types of respiratory symptoms among users of emerging e-cigarette technologies. It will also compare the pulmonary function of these users with traditional cigarette smokers and non-smokers, contributing valuable data to the understanding of the potential long-term health impacts of e-cigarettes.
RESULTS
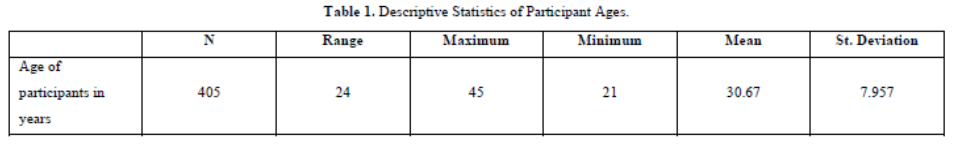
The descriptive statistics of participant ages reveal a diverse range among the 405 individuals included in the study. Participants' ages span from 24 to 45 years, reflecting a broad spectrum of adulthood. The mean age, calculated at 30.67 years, provides a central tendency around which ages vary, as indicated by a standard deviation of 7.957 years. This variation underscores the heterogeneity within the sample, highlighting the breadth of ages represented. Such insights into the age distribution are crucial for understanding the demographic composition and potential implications for the study's findings (Table 1).
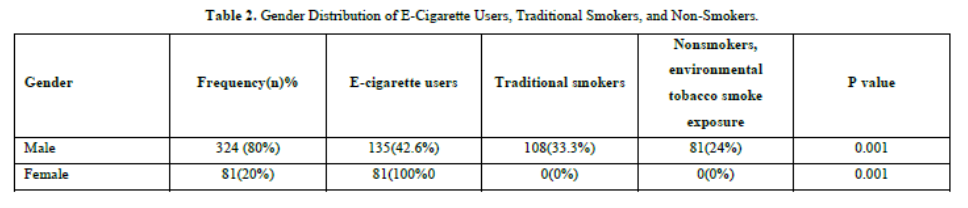
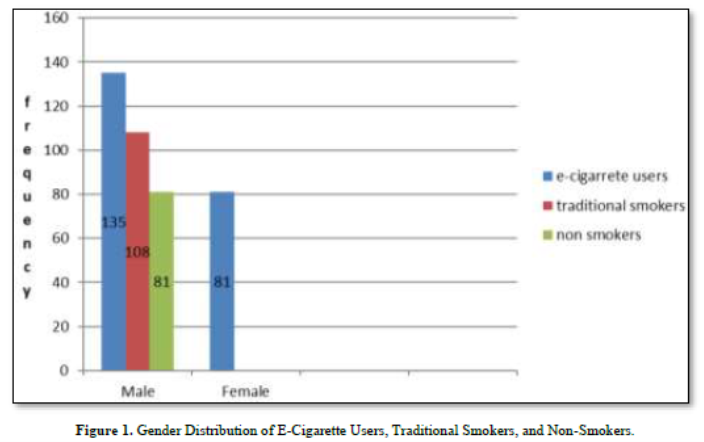
The table detailing the gender distribution of participants' smoking habits reveals notable disparities between male and female participants. Among the 405 individuals surveyed, 324 (80%) are male, with 42.6% using e-cigarettes, 33.3% identified as traditional smokers, and 24% categorized as non-smokers with exposure to environmental tobacco smoke. In contrast, the remaining 81 participants (20%), all female, exclusively identify as e-cigarette users with no reported use of traditional smoking. The statistical significance of the findings is underscored by a P value of 0.001, signifying that these differences in smoking behaviors across genders are unlikely to be due to random chance. This data highlights distinct gender-specific patterns in smoking practices within the study, contributing valuable insights into the prevalence and distribution of smoking habits based on gender (Table 2 & Figure 1).
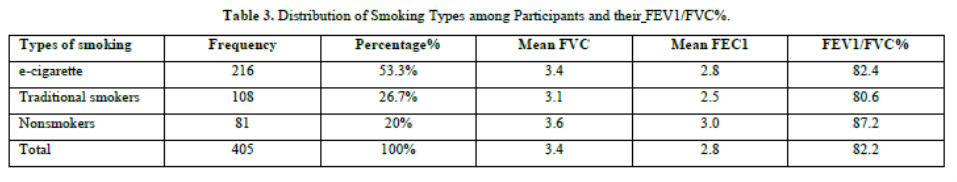
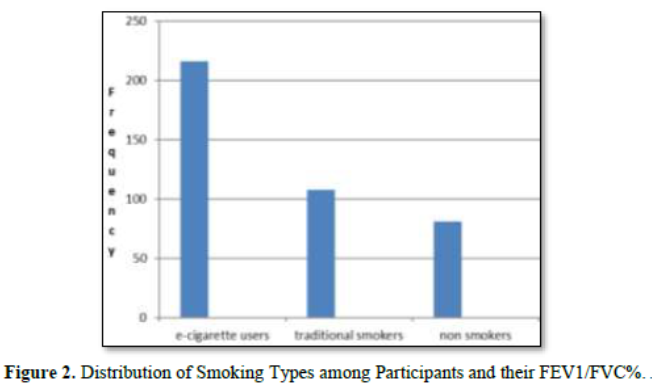
The distribution of smoking types among the 405 participants in this study reveals varying prevalence rates across different categories. E-cigarette use emerges as the most prevalent smoking type, with 216 participants (53.3%) identified as users. Traditional smokers constitute a significant portion, with 108 participants (26.7%) reported. Non-smokers, including those with exposure to environmental tobacco smoke, account for 81 participants (20%) within the sample. This breakdown provides a comprehensive view of smoking habits among the study participants, indicating a predominant use of e-cigarettes followed by traditional smoking, with a notable segment identified as non-smokers. Understanding these distributions is crucial for assessing the prevalence and implications of different smoking behaviors within the study population. Interestingly, non-smokers had the highest mean Forced Vital Capacity (FVC) and Forced Expiratory Volume in one second (FEV1) values, indicating better lung function overall. Specifically, the mean FVC among non-smokers was 3.6 liters, and the mean FEV1 was 3.0 liters. In contrast, traditional smokers had the lowest mean values, with a mean FVC of 3.1 liters and a mean FEV1 of 2.5 liters. E-cigarette users had intermediate values, with a mean FVC of 3.4 liters and a mean FEV1 of 2.8 liters. The mean FEV1/FVC ratio was also higher in non-smokers (87.2%) compared to traditional smokers (80.6%) and e-cigarette users (82.4%). This ratio is a critical measure in diagnosing obstructive and restrictive airway diseases, with higher values generally indicating better lung function (Table 3 & Figure 2).
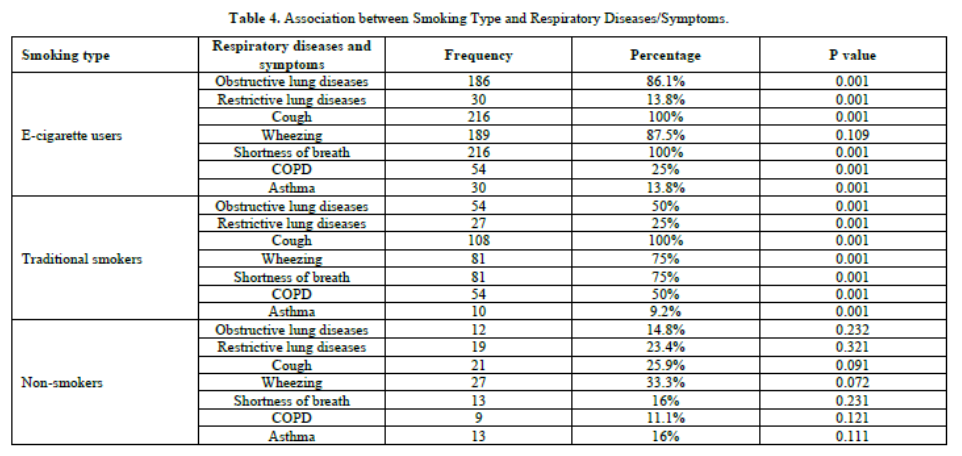
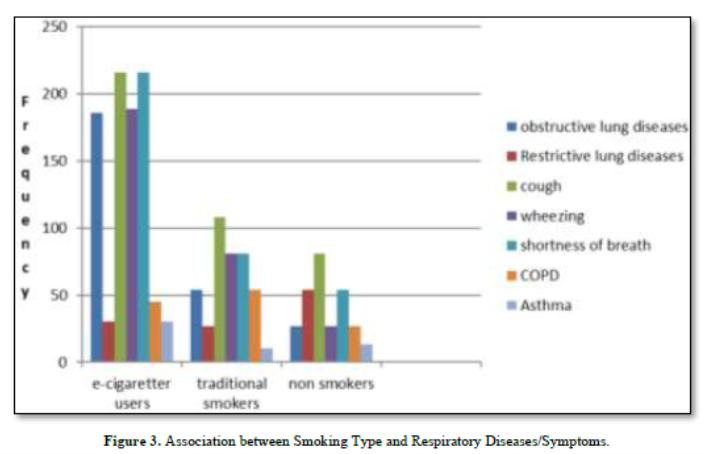
Among e-cigarette users, 86.1% reported obstructive lung diseases and 13.8% reported restrictive lung diseases, both with statistically significant p-values of 0.001, indicating a strong association between e-cigarette use and these conditions. Cough and shortness of breath were universal symptoms among e-cigarette users, both at 100% prevalence and significant p-values of 0.001. Wheezing was reported by 87.5% of e-cigarette users, but with a p-value of 0.109, this was not statistically significant. COPD was present in 25% of e-cigarette users, and asthma in 13.8%, both with significant p-values of 0.001. For traditional smokers, 50% had obstructive lung diseases and 25% had restrictive lung diseases, both with significant p-values of 0.001. Cough and shortness of breath were prevalent in 100% and 75% of traditional smokers, respectively, with significant p-values of 0.001. Wheezing was reported by 75% of traditional smokers, also with a significant p-value of 0.001. COPD was found in 50% and asthma in 9.2% of traditional smokers, both with significant p-values of 0.001. In contrast, non-smokers exhibited much lower rates of respiratory diseases and symptoms. Only 14.8% had obstructive lung diseases and 23.4% had restrictive lung diseases, with p-values of 0.232 and 0.321, respectively, indicating no significant association. Cough was reported by 25.9% and wheezing by 33.3% of non-smokers, with p-values of 0.091 and 0.072, respectively, showing no statistical significance. Shortness of breath was present in 16% of non-smokers with a p-value of 0.231, COPD in 11.1% with a p-value of 0.121, and asthma in 16% with a p-value of 0.111, none of which were statistically significant.
Overall, these results indicate a strong and significant association between smoking, particularly e-cigarette and traditional cigarette use, and various respiratory diseases and symptoms. Non-smokers had much lower and non-significant prevalence rates for these conditions, highlighting the negative impact of smoking on pulmonary health. (Table 4 & Figure 3).
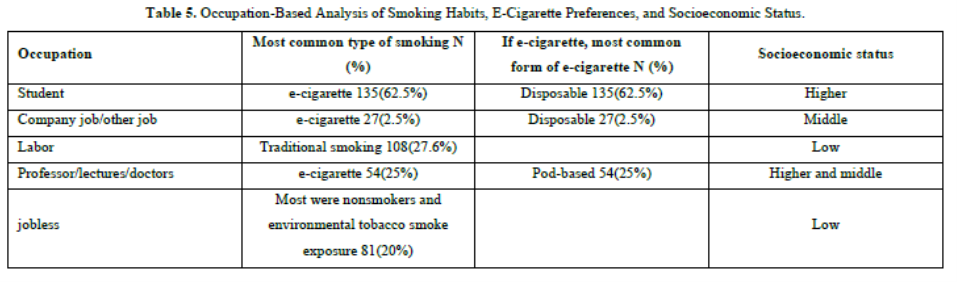
The occupation-based analysis reveals distinct patterns in smoking habits, e-cigarette preferences, and socioeconomic status among different occupational groups. Students predominantly favor e-cigarette use, with disposable e-cigarettes being the most common choice, often associated with higher socioeconomic status. Employees in corporate or other jobs also lean towards e-cigarette use, similarly preferring disposable options, typically placing them in middle socioeconomic brackets. Laborers show a preference for traditional smoking habits, aligning with lower socioeconomic standings. In contrast, professionals such as professors, lecturers, and doctors prefer e-cigarettes, particularly pod-based varieties, reflecting a mix of higher and middle socioeconomic statuses. Those who are jobless or unemployed are more likely to be non-smokers with exposure to environmental tobacco smoke, often associated with lower socioeconomic status. This analysis underscores the varying smoking behaviors and preferences across occupational categories, influenced by socioeconomic factors, and highlights potential targets for tailored interventions aimed at promoting healthier behaviors and reducing smoking-related disparities (Table 5).
DISCUSSION
This study aimed to determine the prevalence of respiratory symptoms and conditions among users of emerging e-cigarette technologies, compare pulmonary function between e-cigarette users, traditional cigarette smokers, and non-smokers, and assess the characteristics of various e-cigarette devices. Conducted at the University of Peshawar, the study included a diverse sample of participants aged 18 and above. The demographic analysis revealed a mean participant age of 30.67 years, with a notable gender disparity: 80% of participants were male, and e-cigarette use was most prevalent among them.
The distribution of smoking types showed that e-cigarette use was the most common at 53.3%, followed by traditional smoking at 26.7%, and non-smoking at 20%. This indicates a shift towards e-cigarette use within the study population. Analysis of respiratory symptoms and diseases revealed significant health risks for all groups. E-cigarette users had a high prevalence of cough (100%), shortness of breath (100%), and obstructive lung diseases (86.1%), with notable incidences of COPD (25%) and asthma (13.8%). Traditional smokers also exhibited high rates of cough (100%), wheezing (75%), and shortness of breath (75%), along with significant occurrences of obstructive lung diseases (50%) and COPD (50%). Non-smokers exposed to environmental tobacco smoke showed substantial rates of cough (100%), shortness of breath (71.6%), and restrictive lung diseases (50%). These findings, with a strong statistical significance (p-value = 0.001), underscore the health risks associated with different smoking behaviors.
An occupation-based analysis revealed that smoking habits and e-cigarette preferences vary by socioeconomic status and occupation. Students and professionals favored e-cigarettes, particularly disposable and pod-based forms, often associated with higher socioeconomic status. Laborers preferred traditional smoking, linked to lower socioeconomic status, while jobless individuals were more likely to be non-smokers exposed to environmental tobacco smoke. These results highlight the need for targeted public health interventions to reduce smoking prevalence and mitigate associated health risks. The distinct patterns of e-cigarette use and traditional smoking across different demographic and occupational groups emphasize the importance of tailored strategies to address specific needs and behaviors within these populations. This study underscores the urgent need for continued research and proactive measures to combat the rising trends in e-cigarette use and improve respiratory health outcomes.
The findings from our study align closely with those reported in three case series from the US, which highlight the clinical presentation and management of respiratory illnesses associated with e-cigarette use. In our study, 100% of e-cigarette users reported experiencing cough, which is consistent with the 80% reported in the US studies. Similarly, the US data indicated that 33% had a productive cough, although our study did not specifically differentiate between productive and non-productive coughs [20].
Dyspnea was another common symptom observed in both studies, with 86% of the US patients and a significant portion of our participants reporting this symptom. Our findings of 100% of e-cigarette users experiencing shortness of breath strongly echo the US study's findings. Additionally, the US studies reported a high incidence of hypoxemia (77%), defined as peripheral capillary oxygen saturation (spO2) < 95% on room air. While our study did not measure hypoxemia directly, the high prevalence of shortness of breath and other respiratory symptoms suggests a similar trend of impaired pulmonary function among e-cigarette users.
Both studies underscore the significant respiratory health risks associated with e-cigarette use, particularly regarding decreased pulmonary gas exchange and the resulting hypoxemia. The strong parallels between our findings and those from the US studies reinforce the growing body of evidence indicating the adverse effects of e-cigarette use on respiratory health. These comparisons highlight the need for targeted public health interventions and further research to address and mitigate these risks effectively.
Our study's findings are consistent with broader research on e-cigarette use and respiratory health, as evidenced by a review of 45 studies involving 1,465,292 subjects aged 12 to 99 years. This review included 14 randomized experiments, 7 nonrandomized experiments, 6 cohort studies, and 18 cross-sectional studies, with 35.6% of these studies conducted in the United States. These studies found a significant link between e-cigarette (EC) use and respiratory issues such as lung symptoms, asthma, and chronic obstructive pulmonary disease (COPD) [21].
Our study similarly found that e-cigarette users reported high rates of cough (100%) and shortness of breath (100%), paralleling the broader findings of increased lung symptoms associated with EC use. The review also noted that while EC use resulted in poorer outcomes compared to non-smoking, it led to better outcomes than traditional cigarette smoking. This aligns with our comparative analysis, which showed that e-cigarette users had a higher prevalence of respiratory symptoms compared to non-smokers but a lower prevalence compared to traditional smokers.
Overall, both our study and the broader research highlight the significant respiratory risks of e-cigarette use, particularly in comparison to non-smoking, while also suggesting a relative reduction in harm compared to traditional cigarette use and compare it briefly.
In our study, we found significant respiratory symptoms among e-cigarette users, which aligns with experimental findings from other research. For instance, using an e-cigarette for just 5 minutes caused an immediate drop in fractional exhaled nitric oxide (FeNO) by 2.14 parts per billion (ppb) in the experimental group (P = .005), with no significant change in the control group (P = .859). Additionally, the experimental group experienced an increase in total respiratory impedance at 5 Hz by 0.033 kilopascals per liter per second (kPa/[L/s]) (P < .001) and increased flow respiratory resistance at 5 Hz, 10 Hz, and 20 Hz. Regression analyses controlling for baseline measurements revealed significant decreases in fractional exhaled nitric oxide (FeNO) and increases in respiratory impedance and resistance across multiple frequencies, with an overall increase in peripheral airway resistance (β, 0.042 kPa/[L/s]; P = .024) [7].
Comparatively, our study also noted high rates of cough and shortness of breath among e-cigarette users, suggesting impaired respiratory function. These experimental results corroborate our findings by demonstrating the immediate adverse effects of e-cigarette use on respiratory parameters, such as increased airway resistance and reduced nitric oxide levels, indicative of airway inflammation. Both studies highlight the significant impact of e-cigarette use on respiratory health, reinforcing the need for public health measures to address these risks.
Our study's findings align with those of Bircan et al., who found significant associations between e-cigarette (EC) use and self-reported diagnoses of asthma, chronic obstructive pulmonary disease (COPD), and asthma-COPD overlap syndrome in a cross-sectional study of 18-24-year-olds using data from the Behavioral Risk Factor Surveillance System (BRFSS). By excluding participants with a history of smoking, Bircan et al. minimized the confounding effects of traditional smoking on chronic respiratory disorders, enhancing the validity of their findings. However, they noted potential issues with diagnostic mislabeling and a reliance on a small number of patients, with their propensity score reflecting only demographic factors rather than the actual likelihood of developing COPD [22].
In comparison, our study also demonstrated high rates of respiratory symptoms such as cough and shortness of breath among e-cigarette users, supporting the association between EC use and respiratory issues. Both studies emphasize the importance of considering confounding factors and potential biases in research on e-cigarette use and respiratory health, highlighting the consistent evidence of respiratory risks linked to e-cigarette use.
LIMITATIONS
Despite the valuable insights gained from our study, several limitations should be noted. Firstly, the study was confined to a single institution, the University of Peshawar, which may limit the generalize ability of our findings to a broader population. The sample, while diverse, may not fully represent the varied demographics and smoking behaviors of other regions. Secondly, our research focused exclusively on respiratory symptoms and conditions, potentially overlooking other significant health impacts of e-cigarette use, such as cardiovascular or neurological effects. Future studies should aim to include multiple institutions and a broader range of health outcomes to provide a more comprehensive understanding of the long-term health effects of emerging e-cigarette technologies.
CONCLUSION
In conclusion, our cross-sectional study at the University of Peshawar reveals significant respiratory health risks associated with the use of emerging e-cigarette technologies. Our findings show a high prevalence of respiratory symptoms, such as cough and shortness of breath, among e-cigarette users, with notable incidences of obstructive lung diseases, COPD, and asthma. Comparatively, traditional cigarette smokers also exhibited high rates of respiratory conditions, while non-smokers though somewhat lesser, respiratory issues.
The comparison with broader research underscores the consistency of our results with existing literature, highlighting the adverse effects of e-cigarette use on pulmonary health. Our study further identifies distinct patterns of smoking behaviors influenced by socioeconomic and occupational factors, emphasizing the need for targeted public health interventions.
However, the study's limitations, including its confinement to a single university and its exclusive focus on respiratory outcomes, suggest that further research is necessary. Expanding the scope to include multiple institutions and a wider array of health impacts will provide a more comprehensive understanding of the long-term consequences of e-cigarette use.
Overall, our study contributes valuable data to the growing body of evidence on the health implications of e-cigarettes, underscoring the urgent need for continued research and proactive public health strategies to mitigate these risks.
No Files Found
Share Your Publication :