-
Publish Your Research/Review Articles in our High Quality Journal for just USD $99*+Taxes( *T&C Apply)
Offer Ends On
Gizem Ecem Kocak Nuhoglu*, Umut Kadir Balci, Tugce Bugce Elbeyi and Hakki Tanyeri
Corresponding Author: Gizem Ecem Kocak Nuhoglu, Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Istanbul Kent University, Istanbul, Turkey.
Received: June 05, 2024 ; Revised: June 09, 2024 ; Accepted: June 12, 2024 ; Available Online: June 28, 2024
Citation: Nuhoglu GEK, Balci UK, Elbeyi TB & Tanyeri H. (2024) A Case Report: Ameloblastic Fibroma. J Oral Health Dent Res, 4(1): 1-5.
Copyrights: ©2024 Nuhoglu GEK, Balci UK, Elbeyi TB & Tanyeri H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Views & Citations
Likes & Shares
Ameloblastic fibroma is a rare benign odontogenic tumor containing epithelial and connective tissue components, usually seen in the 2nd decade. The patient in this article applied to our clinic with the symptoms of pain and numbness that he sometimes felt in his left lower jaw, and a lesion involving teeth number 36-37 and extending up to the mandible ramus was detected in his panoramic x-ray. Teeth 36-37 associated with the lesion were extracted while preserving the mandibular nerve, and the lesion was removed by enucleation + curettage and sent to pathology. According to the pathology results, it was determined that the lesion was ameloblastic fibroma. The patient was followed up regularly for recurrence. In this case report, the ameloblastic fibroma case is described clinically, radiographically and histopathologically, and the possibility of recurrence and treatment protocol are discussed under the literature information.
Keywords: Ameloblastic fibroma, Odontogenic tumor, Ameloblastic fibro-odontoma
INTRODUCTION
Ameloblastic fibromas are one of the rare types of benign odontogenic tumors, made up of proliferative developing odontogenic epithelium settled in cellular ectomesenchymal tissue similar to dental papilla.
They are mostly located in the posterior region of the mandible; The majority of cases are in the area of the second primary molar or first permanent molar and are associated with an impacted tooth [1]. 75% of ameloblastic fibromas cases occur in the second decade, and men are affected 4 times more than women. Ameloblastic fibromas are one of the rare types of benign odontogenic tumors, made up of proliferative developing odontogenic epithelium settled in cellular ectomesenchymal tissue similar to dental papilla. They are mostly located in the posterior region of the mandible; The majority of cases are in the area of the second primary molar or first permanent molar and are associated with an impacted tooth [1]. 75% of ameloblastic fibromas cases occur in the second decade, and men are affected 4 times more than women. Since the lesion is asymptomatic, most cases are diagnosed on radiological examination. It can be seen as unilocular or multilocular on radiography. While unilocular lesions are asymptomatic, swelling and pain may occur in multilocular lesions. Relapse rates are low. Although radical surgical approaches are applied in advanced lesions, curettage and enucleation are also used. It is frequently applied [2].
CASE REPORT
An 18-year-old female patient applied to our clinic with complaints of mild pain and paresthesia in her left lower jaw. As a result of the radiographic examinations (panoramic radiography, CT scan), a radiolucent, well-defined, non-expandable, two-compartment lesion was detected in the left posterior region of the patient's mandible, extending from the apical of tooth number 36 to the ramus. It was observed that the lesion, in which tooth number 37 was impacted at the apical part of tooth number 36, pushed the mandibular nerve inferiorly. There is no facial asymmetry or loss of function in the clinical examination of the patient. A biopsy was taken from the patient under local anesthesia and sent for pathological examination. As a result of the pathological report, it was determined that the lesion was Ameloblastic Fibroma. The patient was operated on under general anesthesia.
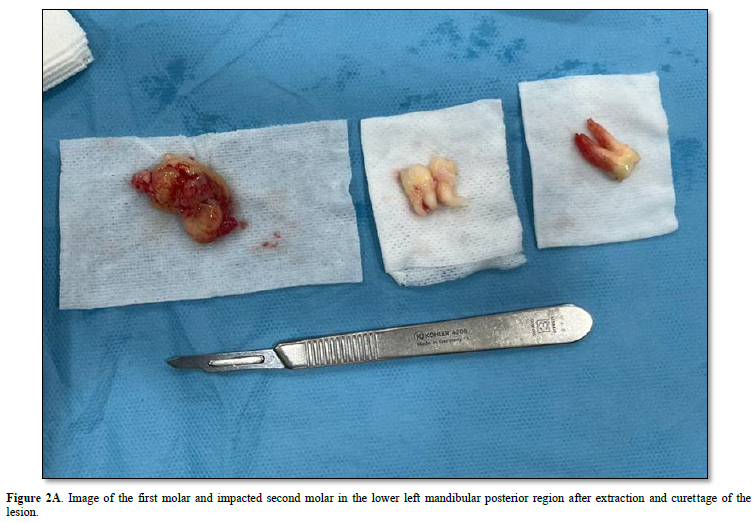
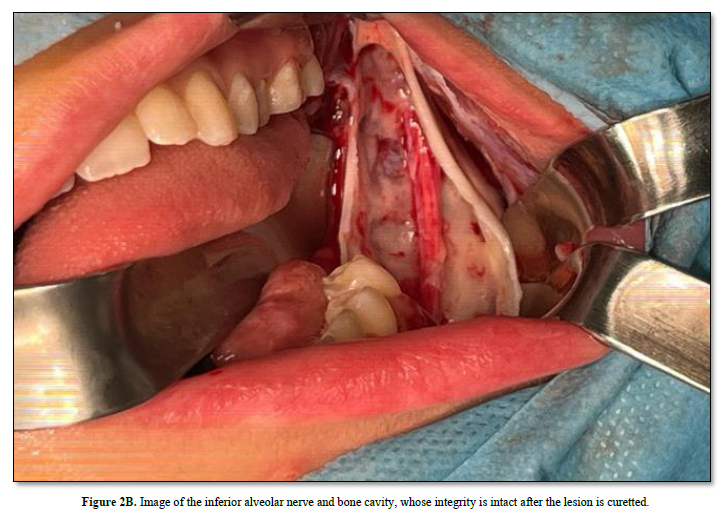
After local anesthetic agents were applied to the lesion area, a winter-style intraoral incision was made from the mesial of tooth number 34 to the margo anterior region of the ramus with the help of a scalpel. A full-thickness mucoperiosteal flap was raised and the lesion was accessed. Tissue with mucous consistency, myxoid structure and no bleeding was enucleated. Tumor-related teeth 36 and 37 were extracted while preserving the mandibular nerve. The obtained specimen was sent for pathological examination again for confirmation. The surgical area was closed primarily with 4-0 pegalac suture.
The tumor, whose microscopic features are defined in the second pathology report comment, has microscopic features of odontogenic fibroma, ameloblastic fibroma, odontogenic myxoma, ameloblastoma, primodial odontogenic tumor, odontoma, odontoameloblastoma, ameloblastic fibrodentinoma, ameloblastic fibro-odontoma and many similar tumors. Since both mesenchymal and epithelial components are very prominent and also contain three types of epithelium, the diagnoses of odontogenic myxoma, odontogenic fibroma, ameloblastoma, ameloblastic fibroma and primordial odontogenic tumor have been moved away. Although it resembles an odontoma, containing predominantly pulp, dentin and enamel tissues, the epithelial component in this tumor is much more exaggerated than that seen in odontoma and hard tissues are minimal. The histomorphological findings of the tumor overlap with the diagnostic features of odontoameloblastoma, ameloblastic fibrodentinoma, and ameloblastic fibro-odontoma, which are described in the sources but not in the WHO (2017) classification. These tumors are tumors with similar morphologies that are used interchangeably in the old WHO classification and other classifications, and the exact distinction between them has not been determined.
In the latest classification, WHO removed ameloblastic fibro-odontoma from the classification, considering it as an intermediate developmental stage of a tumor developing from ameloblastoma to odontoma. In this case, considering that we examined the entire tumor and that the dental hard tissue is seen in a very small focus and that fibroma and odontogenic-ameloblastic epithelium are determinants of morphology, it can be said that the prognostic process will be compatible with "Ameloblastic Fibroma" (Figures 1-3).



DISCUSSION
Ameloblastic Fibroma is part of a group called mixed odontogenic tumors, which includes Odontoma and Odontoameloblastoma. The literature classification on this topic is confusing. One of the areas of debate is the difference between AFO in terms of neoplasia and hamartoma [3].
The term ''epithelial odontogenic tumor containing odontogenic mesenchyme'' is now more widely accepted and avoids potential controversy over the nature of the neoplasia. The term ''AFO'' represents the histological combination of ameloblastic fibroma and complex odontoma. This lesion exhibits the same benign biological behavior as ameloblastic fibroma. In contrast, the term ''ameloblastic odontoma'' refers to tumors that represent a histological combination of ameloblastoma and complex odontoma and behave in the invasive manner of classical ameloblastomas.
The most common complaints are swelling and inflammation in the wrong area. The lesion may displace erupted teeth, but other symptoms such as pain and paresthesia are rare. Asymptomatic cases are often discovered incidentally on radiography. Rarely, the tumor results in significant swelling, causing facial disfigurement [4].
Many authors have reported that AFO is non-aggressive and can be adequately treated by surgical curettage without extraction of adjacent teeth [5]. Dhanuthai [6] recorded the case of a 1-year-old child with AFO who was treated with enucleation and did not relapse at 1-year follow-up [6]. Additionally, Howell and Burkes presented two cases of malignant transformation of AFOs; They stated that malignant transformation of ameloblastic fibromas, ameloblastic odontomas and AFOs is more common than previously thought [7]. Bregni and colleagues [8] previously reported ameloblastic fibrosarcomas developing from benign tumors such as AFO.
CONCLUSION
The purpose of this case report is to share our experience in the treatment of a rare case of ameloblastic fibro-odontoma. AFO exhibits varying clinical and radiographic features, and its diagnosis is confirmed only by histological examination. Some authors say that ameloblastic fibro-odontoma and complex odontoma are different pathologies, while some authors state that they are different stages of the same pathology. Considering that ameloblastic fibro-odontoma has low recurrence, benign behavior and minimally invasive nature, the first treatment is tooth extraction and curettement of the lesion. In this case, the integrity of the inferior alveolar nerve was preserved during curettage.
Potential transformation alone does not justify radical treatment of all these benign lesions. As noted in the literature review, not all lesions previously classified as AFOs are aggressive lesions and should not be expected to recur following conservative surgical intervention. When relapse occurs, accompanied by changes in the histological pattern towards a more disorganized fibrous stroma with displacement of the epithelial component, more extensive treatment procedures are indicated.
No Files Found
Share Your Publication :