-
Publish Your Research/Review Articles in our High Quality Journal for just USD $99*+Taxes( *T&C Apply)
Offer Ends On
Thai Yeng*
Corresponding Author: Thai Yeng, BDS, MDentSci, DClinDent, PhD, MRACDS (Endo), MRCPS (Glasg), FDSRCPS (Glasg), FDSRCS (Edin), FDSRCS (Eng), FPFA, Specialist Endodontist, North Sydney Dental Specialist, Sydney, NSW, Australia.
Received: March 10, 2023 ; Revised: March 14, 2023 ; Accepted: March 17, 2023 ; Available Online: March 31, 2023
Citation: Yeng T. (2023) Late Failure in Endodontic Treatment: An Exemplar Case Study. J Oral Health Dent Res, 3(1): 1-5.
Copyrights: ©2023 Yeng T. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Views & Citations
Likes & Shares
This exemplar case highlights the potential factors contributing to the late failure of an endodontically treated mandibular first molar successfully treated five years ago. Late failures in endodontic treatment may be viewed as the appearance or reappearance after healing of radiographic evidence of apical periodontitis, with or without associated clinical signs or symptoms of reinfection of the root canal system occurring some years later.
Clinical relevance: It is possible that initially healed cases of endodontically treated teeth could later become unsuccessful. Factors other than the root canal treatment itself may contribute to late failures.
Aim: To identify potential causative factors that may contribute to late failure of successful endodontically treated cases some years later.
Keywords: Root canal treatment, Root canal retreatment, Coronal leakage, Intra-radicular infection, Root fracture
INTRODUCTION
When root canal treatment is adequately carried out, healing of the periapical lesion usually occurs with a gradual reduction and resolution of the radiolucency observed on subsequent examination [1,2]. To assess the outcome of root canal therapy, a long-term radiographic and clinical review is essential [3]. The European Society of Endodontology has suggested that root canal treatment should be followed for a minimum period of 4 years [4]. If a lesion is detected after 4 years, then this may be considered to be associated with post treatment disease [4].
Root canal treatment usually fails when the treatment is performed inadequately [5], but in certain cases, failure is seen despite the highest standard of treatment [6]. From a biological perspective, an endodontic failure is associated with an inflammatory process in the periradicular area of the tooth [7]. Most authors highlight Enterococcus faecalis as the main microorganism associated with endodontic failure [8]; however, recent studies have isolated, other bacteria, such as Fusobacterium nucleatum and Propionibacterium, to a greater extent [9].
Endodontic failures cluster into early and late failures [10,11]. Early failures usually result from the inadequate root canal therapy performed by the clinician, with symptoms arising soon after initial treatment [3]. Late failures, however, tend to involve factors other than the root canal therapy itself [12], such as recontamination of the root canal system via coronal leakage [13], root fractures [14], and the possibility of intra-radicular infection [15].
The aim of this paper is to present an exemplar case of a late failure in endodontic treatment and identify potential causative factors contributing to the loss of the tooth many years later.
CASE REPORT
A 43-year-old patient was referred for management of their lower left first molar (LL6) in 2017. In 2016, the patient had a root canal treatment and crown provided by his general dentist. Soon after completing the initial endodontic treatment, the patient complained of discomfort, with pain arising from the tooth when biting on food and then a throbbing ache that would last for a few minutes. The patient also presented with fluctuating buccal swelling. The patient was not keen to have LL6 extracted, especially since the completed root canal therapy was within 12 months, and instead wished to try to prolong the survival of LL6 with endodontic retreatment. Although dental implant was an option, the patient preferred to avoid having a fixed or removable prosthesis for financial reasons.
The following clinical and radiographic information was recorded by the endodontist during the consultation for LL6. Clinical findings included tenderness to percussion, pain on palpation around the periapical area, and fluctuant buccal swelling. There was an absence of any sinus tract on the labial or lingual aspect, and normal periodontal health with no deep pocketing was detected. In addition, no caries was detected, normal tooth mobility was observed, a negative Fracfinder test resulted, and there was no clinical evidence of coronal leakage around the existing new crown.
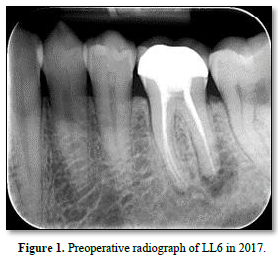
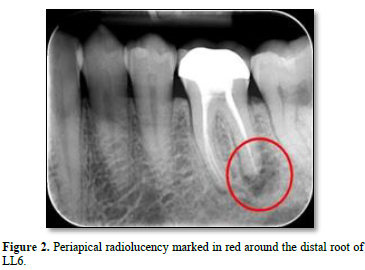
Radiographic findings included periapical radiolucency around the distal root of LL6, as shown in Figures 1 & 2, with no furcal or angular bone loss. Additionally, no caries or cavitation of the tooth structure or evidence of an open defect around the crown were detected; and the technical standard of the root canal filling appeared acceptable, with no procedural complications identified on the radiographs.
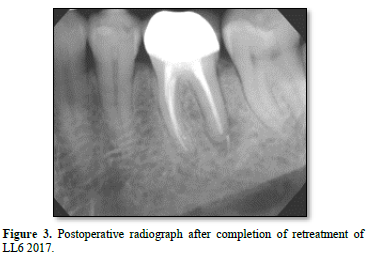
The endodontist’s provisional diagnosis was a symptomatic apical periodontitis associated with an infected root canal system of LL6. Endodontic retreatment commenced, under rubber dam isolation with the removal of the old root canal fillings and instrumentation to the working lengths, as determined by the apex locator. Calcium hydroxide medicament was used, and no evidence of cracks, fractures, or caries was seen with a dental operating microscope. The isthmus between the disto-buccal and disto-lingual canals was found to contain infected tissue debris; this was suspected to be the principal cause for the early failure of the original endodontic treatment. Retreatment of LL6 was completed after a period of intracanal medicament dressing and was root-filled 3 months later wherein a slight sealer extrusion was noticed beyond the distal root, as shown in Figure 3.
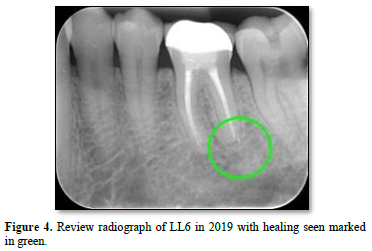
The patient returned to his general dentist for routine dental maintenance and was reviewed again by the endodontist in 2019. The original periapical radiolucency around the distal root had resolved (as shown with the green circle in Figure 4, and the LL6 continued to be asymptomatic and clinically stable.
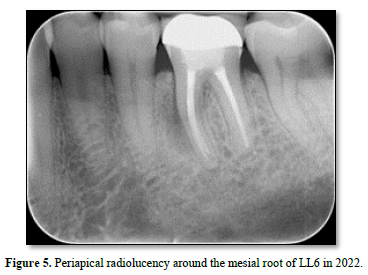
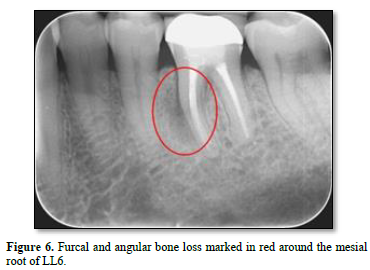
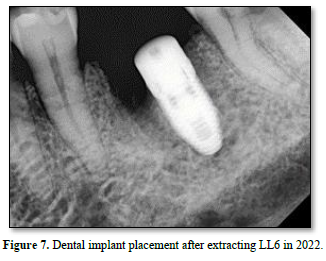
In 2022, however, the patient complained of a buccal swelling that had developed around LL6. The patient now could not bite on any type of food, and a throbbing ache was experienced whenever he applied pressure to the tooth with his tongue. A deep, narrow periodontal pocket of 10 mm was detected along the mesial buccal root. A mid-root periapical radiolucency is seen along the mesial root, as shown in Figure 5. Both angular and furcal bone loss were evident on the radiograph, as shown in Figure 6. A defect around the crown is now clinically detectable, with recurrent decay suspected as a gap around the crown was now open to the oral cavity. However, the original infection site around the distal root remained healed after retreatment. Based on supporting clinical and radiographic evidence, a vertical root fracture (VRF) of LL6 was suspected. Alternative diagnoses were considered, including a periapical abscess, periapical granuloma, periapical cyst, cracked tooth, and a periodontal-endodontic combined lesion. After a lengthy discussion, the patient consented to having LL6 extracted by a specialist oral surgeon, and a VRF was confirmed. A dental implant was then placed into the extraction site by the specialist oral surgeon as shown in Figure 7.
DISCUSSION
This case exemplar showed an initially healed early failure root canal following endodontic retreatment in 2017, becoming unsuccessful approximately five years later. Factors contributing to the development of late failure may include coronal leakage, new fractures, and latent intra-radicular infections. Several long-term clinical studies [10,12,29] support the importance of longer periods of review (longer than 4 years as suggested by the European Society of Endodontology) [4] to detect any late failures following endodontic therapy. This exemplar supports this conclusion.
Coronal leakage is an important factor that may contribute to the failure of good endodontic treatments by allowing microorganisms to contaminate the obturated root canals [13]. Both in vitro laboratory experiments [16] and in vivo animal studies [17] indicate the possibility of bacterial leakage contaminating the root canal system and ultimately leading to treatment failure at a later time. In this exemplar case, a gap was detected clinically around the existing crown margins in 2022; this was not seen in 2017 nor confirmed on the radiograph (Figure 1). This may implicate bacterial leakage from oral fluids and contamination of the root canal system.
The literature review Heling [18] conducted between 1969 and 1999 suggested that once the coronal seal is lost, bacteria and other irritants from saliva may reach the periradicular tissues, affecting the outcome of the root canal therapy. The absence of periapical infection around an endodontically treated tooth in the long term is dependent on good quality coronal restoration and a well-performed root canal treatment combined [19,20]. Ricucci and Bergenholtz [21], however, challenged the significance of coronal leakage. Their observations concluded that good endodontic treatment, involving adequate chemomechanical therapy and an optimal root canal filling, could resist bacterial leakage even when coronal restoration is inadequate or lost. Their results showed that bacterial penetration of the root canal fillings mainly affected the coronal portion of the root canal, even after exposure to bacteria and caries for a prolonged period. If root canal treatment was inadequate, subsequent coronal leakage may result in disease recurrence and, ultimately, late failures.
Development of a new fracture can lead to the loss of a good endodontically treated tooth. Vire [14] observed that close to half of the failures seen over a 1-year period in endodontically treated teeth treated in a busy group practice were due to crown fractures, and the average time between completion of endodontics and extraction was 59.4 months. This finding agrees with Salehrabi and Rotstein [11]. Their retrospective study over an 8-year period on the outcome of initial root canal treatment showed that nearly 80% of the extracted teeth recorded during the period did not have a crown. This is unsurprising since studies have shown that full coronal coverage is important to the long-term outcome of endodontically treated teeth [10,22]. To prevent root canal treated teeth from fracturing, a retrospective cohort study by Aquilino and Caplan [23] observed a strong association between crowns as a coronal restoration and the long-term tooth survival of root canal-treated teeth [23]. A crown restoration that provides full cuspal coverage ideally should protect the endodontically treated tooth against fracture [22,24]. This exemplar case, however, developed a vertical root fracture even though the tooth was crowned, that ultimately required extraction. Therefore, this case could be interpreted as a late endodontic failure.
Intra-radicular infections are a major causative factor leading to the failure of both adequate and inadequately endodontically treated teeth [6]. With bacteria harboring in the anatomical complexities of the root canal system, inaccessible to chemomechanical therapy [3], the intra-radicular bacteria multiply and become pathogenic if nutrients are available (e.g., as in coronal leakage) [25] and eventually play a role in late endodontic failures. The presence of the bacteria in the root canal system could be due to residual flora from the original infection, being introduced during root canal therapy appointments, or having invaded the root canal system following post-treatment via coronal leakage [26]. Bacteria within the root canal system could play an essential role in the pathogenesis of periradicular lesions if they possess pathogenicity, reach sufficient numbers, and communicate with the periradicular tissues [6]. Chavez de Paz [27] recovered non-mutans streptococci, enterococci, and lactobacilli after antimicrobial endodontic therapy in teeth with apical periodontitis. These microorganisms persisted after chemomechanical procedures and could have a role in supporting the pathological process and maintaining apical periodontitis. Adib [28] also agreed with the findings of Chavez de Paz [27] when they identified both streptococci and enterococci in endodontically treated teeth with persisting apical periodontitis and coronal leakage. In my view, in this exemplar case a few bacterial species could have survived the chemomechanical retreatment procedures and, with further bacterial ingress from either coronal leakage or via the fracture line along the root, communicated with the periradicular tissues to establish a periapical infection, thus resulting in the late failure of this endodontically treated case.
Long-term clinical studies have reported that late failures in endodontics can be observed after longer review periods. Cheung and Chan’s [10] observation of endodontically treated teeth over long periods - i.e., between 10 and 20 years following initial root canal treatment showed two different rates of decline in the survival of endodontically treated teeth. An initial fast decline was observed before the 18-month postoperative period, and a slow non-linear decline was seen after the 18-month period. The initial rapid rate of decline could indicate early failures, which usually reflect the inadequacy of the treatment in controlling the root canal infection. The slower, non-linear decline could imply late failures. Hayes and Drummer [12] reported a case in which failure of root canal treatment was observed 17 years following initial treatment. Although this was a case report and the level of evidence does not score highly compared to a randomized controlled clinical trial, it illustrates the concept of late failure after a period of non-eventful healing. Molven [29] reported, however, that for the periods between 20 and 27 years following initial root canal treatment, only 1.5% of endodontically treated teeth developed periapical radiolucency. The late development of periapical lesions could be due to an intra-radicular infection where bacteria in the root canal system had been dormant or in reduced numbers for some period [6], or bacterial ingress via coronal leakage [13,20] indicating late failures. To reduce the risk of late failures, prompt restoration after root canal treatment is crucial to the long-term survival of endodontically treated teeth [30]. In this exemplar case, late failure was observed after 5 years of review, implying the importance of longer observation periods.
CONCLUSION
Late failures in endodontic treatment may be viewed as the appearance or reappearance after healing of radiographic evidence of apical periodontitis, occurring some years later. Late failures could be attributed to a variety of causes involving factors other than the root canal therapy itself. These include reinfection of the root canal system by coronal leakage, fractures that lead to new infection of the root canal system, and the possibility of latent intra-radicular infection when microorganisms possess pathogenicity or reach a population high enough to induce development of a periradicular lesion. Good root canal treatments sometimes fail over the course of time, contrary to our wishes and best efforts. These situations are viewed as late failures in endodontics.
No Files Found
Share Your Publication :