-
Publish Your Research/Review Articles in our High Quality Journal for just USD $99*+Taxes( *T&C Apply)
Offer Ends On
David Francis Olebo*, Enos Mirembe Masereka, Brenda Night Muhindo, Jacqueline Nalikka and Mubaraka Kayiira
Corresponding Author: David Francis Olebo, KOMASE Ebenezer Research Centre Limited, (KoNET), Makerere University Walter Reed Project, Makerere University Walter Reed Project Plot 42, Nakasero Roads P.O. Box, 16524, Kampala, Uganda.
Received: November 28, 2023 ; Revised: December 17, 2023 ; Accepted: December 20, 2023 ; Available Online: January 04, 2024
Citation: Olebo DF, Masereka EM, Muhindo BN, Nalikka J & Kayiira M. (2023) Assessing Partograph Quality and its Impact on Neonatal Outcomes: A Study at Fort Portal Regional Referral Hospital, Uganda. J BioMed Adv Clin Res, 2(1): 1-14.
Copyrights: ©2023 Olebo DF, Masereka EM, Muhindo BN, Nalikka J & Kayiira M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Views & Citations
Likes & Shares
The partograph is a tool used to monitor labor progress to detect early dangers such as prolonged and obstructed labor, enabling timely referral and interventions to safeguard the well-being of both the mother and the baby.
Globally, the maternal mortality ratio (MMR) stands at 158.8 deaths per 100,000 live births, with projections indicating a decrease to 140.9 deaths per 100,000 live births in 2030 and an annual 2.5 million neonatal deaths, primarily occurring in low- and middle-income countries. These mortalities can largely be attributed to inadequate monitoring of mothers during labor. This study explored the quality of partographs used by midwives at Fort Portal Regional Referral Hospital (FPRRH), along with their associated outcomes, and measured the connection between partograph quality and these outcomes. The aim was to formulate strategies for recommendations to stakeholders.
The methodology employed in this study was a retrospective cross-sectional design that used quantitative approaches. It involved the review of 323 partographs of mothers who gave birth at FPRRH from March 2022 to March 2023.
The findings indicate that the majority of the reviewed partographs were of poor quality, accounting for 70.9%, while 29.1% were classified as good quality partographs. In terms of the general labor outcome, 78% of the neonates were born alive, while 22% experienced stillbirths and early neonatal deaths. Notably, 99.7% of neonates who did not survive had poor-quality partographs. Furthermore, neonates monitored with poor-quality partographs had an Adjusted Odds Ratio (AOR) of 1.011 for mortality, and this was statistically significant with p<0.001.
In conclusion, the quality of the partographs in the hospital was notably low, and there was a significant association between partograph quality and neonatal labor outcomes.
The following recommendations are proposed: Healthcare providers should receive additional training and support to improve the maintenance of accurate and complete partograph records. Implement regular audits and quality improvement initiatives to ensure consistent high-quality partograph documentation and monitoring. Further research is needed to explore the specific factors contributing to the disparities in partograph quality and their impact on neonatal outcomes.
Keywords: Uganda, Fort portal, Partograph quality, Neonatal outcomes, Correlations
Abbreviations: SSA: Sub-Saharan Africa; MMR: Maternal Mortality Ratio; SDG: Sustainable Development Goal; HMIS: Health Management Information Systems; FPRRH: Fort Portal Regional Referral Hospital; RRHs: Regional Referral Hospitals; MOH: Ministry of Health; WHO: World Health Organization; KoNET: Komase Ebenezer Research Centre Limited
INTRODUCTION
Partograph is a tool used to monitor labor progress in order to help detect early dangers like prolonged and obstructed labor so that referral or other interventions can be undertaken to save the mother and the baby [1].
Globally, the maternal mortality ratio (MMR) in 2021 was 158.8 deaths per 100,000 live births, compared to 157.1 deaths per 100,000 live births in 2020. The trajectory projects 140.9 deaths per 100,000 live births in 2030, which is double the Sustainable Development Goal (SDG) target of less than 70 death per 100,000 live births in 2030. However, there are likely subnational variations in MMR, highlighting the need for continued focus on ensuring equitable access to high-quality care and lifesaving interventions during childbirth such as paragraph monitoring of the mothers which is simple to use, cost effective and enables early identification of complications during labor [2]. Although the use of the partograph would have been a cheap intervention it’s not routinely done appropriately in labor wards and it has led to every one in ten mothers dying during labor without proper establishment of the cause and management these has resulted to annual 2.5 million neonatal death, majorly occurring from low- and middle-income countries [3].
In developed countries, studies suggest quality better outcome of labor and proper use of the partograph for example studies in Europe suggest <30 death per 100,000 live birth attributed to proper use of the partograph in monitoring labor [4]. In the United States, according to the National Vital Statistics System of 2020, the maternal mortality ratio was 23.8 deaths per 100,000 live births compared with a rate of 20.1 in 2019 with non-Hispanic Black women having 55.3 deaths per 100,000 live births contributing to its large maternal mortality which is also attributed to inadequate monitoring of the mothers with the partographs during labor among other factors in the health facilities serving the black population [5].
In Sub-Saharan Africa (SSA) by 2030, for every 100,000 live births, an estimated 390 women will die in childbirth. To reach the SDG target, SSA will need an 86% reduction which is an unrealistic feat at the current rate of decline if adherence to route partograph use is not done [6]. According to the study conducted in West Shoa Zone, central Ethiopia in 100 health institutions, the partograph was used routinely by 31.1% of 1376 obstetric care providers [7]. In a systematic review of 38 studies conducted in Sub Saharan Africa that reported 11 427 maternal deaths, twenty-one of the thirty-eight studies were retrospective record reviews with the leading causes of death been obstetric hemorrhage 28.8% attributed to not routinely monitoring the mothers using the partograph [8]. In another study in the region showed a neonatal mortality of 18.6% that is 186 death per 1000 live births attributable to poor monitoring of the mothers in labor with a partograph [9].
In Uganda the average maternal mortality ratio was 328 per 100,000 live births with direct obstetric causes contributed 73.8% of maternal deaths; the most common were hemorrhage 42.7% and sepsis 24.0% pointing to inadequate monitoring of the mothers during labor using the partograph [10]. For neonatal mortality, the country stands at 19 deaths per 1000 live birth. However, with bigger disparities; in rural areas 30 deaths per 1000 live birth, in urban areas 31 deaths per 1000 live birth, in poorest households 26 deaths per 1000 live birth and among the richest household 34 deaths per 1000 live birth. This high proportions in all the listed categories point a gap in quality of monitoring of the mothers in labor using the partographs [11]. In one of the studies conducted in Kamwenge district one of the best performers in maternal and child care in Uganda the use of the partograph that met quality standard criteria for monitoring mothers in labor was 67.9% [12]. In another study conducted in Mulago National Referral Hospital among the 355 Partographs reviewed, over 50% of them were incomplete in key findings and factors associated with poor quality outcome of the partographs were; overwhelming numbers of expectant mothers, other staff responsibilities, Congestion in the maternity ward, The availability of other monitoring tools, limitation in skills, inadequate equipment and supplies, and the state of the mother’s arrival to the hospital [13].
In Uganda the quality of the partographs used to monitor mothers in labor in hospitals range from 2.1 % to 69.9% [12].
In Fort Portal Regional Referral Hospital (FPRRH) which is the third highest in all causes of mortality in all the 15 Regional Referral hospitals (RRHs) in Uganda between 2020 and 2021 with the mortality ranging from 300 to 550 deaths per 10,000 admissions [14]. FPRRH has a culture of carrying out both maternal and neonatal death audits. However, there are no documented measures that have been put in place to improve the quality of the partographs during monitoring of the mothers in labor. If nothing is done mothers will continue being at risk of prolonged labor, obstructed labor and uterine raptures hence increasing the risk of maternal death and neonatal death. This will have an impact for Uganda to achieve the sustainable development goal (SDG) 3 in 2030. There is need therefore to have in depth review of the partographs to identify incomplete parameters with the goal of establishing the quality of the partographs, newborn outcomes of labor and the association of quality of the partographs and outcomes of Labour in FPRRH with the aim of coming up with strategies to be recommended to stakeholders that would enable Uganda a achieve the SDG 3.
MATERIALS AND METHODS
Study Location
The study was conducted at Fort Portal Regional Referral Hospital (FPRRH), situated in Fort Portal Tourism City, Uganda. This hospital encompasses various specialized units, including the Isolation Unit, Mental Unit, Imaging Unit, Pediatrics Department, Medical Department, Surgical Department, Obstetrics and Gynecological Department, Outpatient Department, and the Laboratory Department.
FPRRH serves as a vital healthcare institution, offering both inpatient and outpatient services to residents from 11 districts in the southwestern part of Uganda. These districts include Kyenjojo, Kagadi, Kamwenge, Kibaale, Kasese, Bundibugyo, Kabarole, Kyegegwa, Ntoroko, Bunyangabu, and Kitagewenda. The hospital is staffed by a diverse range of healthcare professionals, including pediatricians, physicians, surgeons, gynecologists, psychiatrists, pharmacists, medical doctors, clinical officers, anesthetists, physiotherapists, nutritionists, laboratory technologists, nurses, and midwives, totaling 430 healthcare workers. With a bed capacity of 333 beds and the hospital on averages deliveries 550 mothers monthly.
Geographically, FPRRH is situated within the city of Fort Portal, approximately 148 kilometers (92 miles) west of Mubende Regional Referral Hospital by road. Furthermore, it is approximately 294 kilometers (183 miles) west of Mulago National Referral Hospital, which is located in Kampala, Uganda's capital and largest city.
Study Design and Setting
The retrospective cross-sectional Study design was used with quantitative approaches used to collect data on the quality of the partographs and neonatal outcomes. The data on quality of the partographs and outcome was collected retrospectively from partographs and charts that were used to monitor the mothers in labor in FPRRH Maternity Unit from 01st March 2022 to 31st March 2023.
Study Population
The study targeted all partographs for women who delivered in FPRRH Maternity Unit from 01st March 2022 to 31stMarch 2023 for the period of 12 months.
Data Collection Tools
This study adapted and modified the partograph audit tool developed by the Uganda ministry of health to come up with the data abstract checklist and had three subsections, first was section for socio-demographic and obstetrical variables of the mother, second section quality of the partograph assessment, and the third section outcome of labor for both the mother and the baby. Data abstraction checklist forms were filled out for each partograph sampled during retrospective chart reviews. The tool was double-checked in real-time for any erroneous entries.
Sample Size and sampling Technique
The study used Kish & Leslie 1965 formula to come up with sample size of 323 with margin of error 5% and 95% confidence interval. For the partographs that were reviewed in this study for their quality and neonatal outcome, we arranged the 6,621 delivery charts that occurred in the period of march 2022 to march 2023 and a coded them numbers the first mother that was delivered on 01st March 2022 was coded 1, second delivery coded 2 and the last delivery on 31st March 2023 was coded number 6,621. We used systematic sampling method to select the partographs that were reviewed. However, simple random sampling was used to pick the first partograph from the pool. We selected the charts for review from the pool of 6,621. The dye was casted and the number that appeared was a six, we reviewed every 6th chart from the sampling frame of 6,621 charts till the sample size of 323 was reached.
The measurements of Variables
The level of Utilization of the Partograph was defined as the percentage of mothers in first stage of labor that were monitored using a partograph. The numerator was the number of partographs for mothers in the first stage of labor that were monitored using a partograph and, the denominator was the entire sample size of the study.
Quality of partograph was assessed by 13 variables (No “0” and Yes “1”). These are assessment of the mother for potential risk factors (Yes or No); recording of Fetal heart rates every half hour (Yes or No); recording of the intactness or rupture of membranes (Yes or No); recording of liquor color upon rupture of membranes (Yes or No); recording of Fetal head molding (Yes or No); recording of cervical dilation every 4-hourly (Yes or No); recording of uterine contractions every half hourly (Yes or No); recording of Fetal descent very 4-hourly (Yes or No); recording of maternal temperature every 4-hourly (Yes or No); recording of maternal pulse rate every half hourly (Yes or No); recording of maternal blood pressure every 4-hourly (Yes or No); urine testing for proteins (Yes or No) and; a recording of actions taken when needed (Yes or No). The overall score was therefore range from 0-13. In computing quality of partograph, any partograph with overall score of 0-10 and 11-13 was regarded as poor and good quality respectively. The percentage of quality partograph in monitoring labor was computed as the number of partographs with respective scores divided by the total number of partographs used.
The general fetal labor outcome in this study is whether the neonate was Alive or Dead.
Data Analysis
Data analysis was performed using SPSS version 20.0, utilizing logistic regression modeling, variables underwent bivariate analysis to establish the correlations between Independent variables and dependent variable and all variables with a correlation with P≤0.05 were subjected to multivariate analysis. The Chi squared test, Odds ratios (OR), and P Values were used to determine measure of associations. The level of significance was set at P≤0.05.
ETHICAL CONSIDERATION AND QUALITY CONTROL
The study approval was secured from Mountains of the Moon University Research Committee, and informed consent to review the partograph charts was also obtained. Confidentiality was diligently upheld throughout the study period. The research assistants involved in the study underwent Human Subject Protection (HSP) and Good Clinical Practice (GCP) training prior to their engagement.
To ensure the reliability and validity of the study, several quality control measures were implemented. These measures included pre-testing the tools, training research assistants in the protocol, and implementing data cleaning and editing procedures. The collected data was stored with restricted access, limited solely to the study team.
Overall, the study adhered to rigorous ethical standards and quality control practices, affirming the integrity and credibility of the research findings.
RESULTS
Socio demographic Characteristics of mothers whose partographs were studied
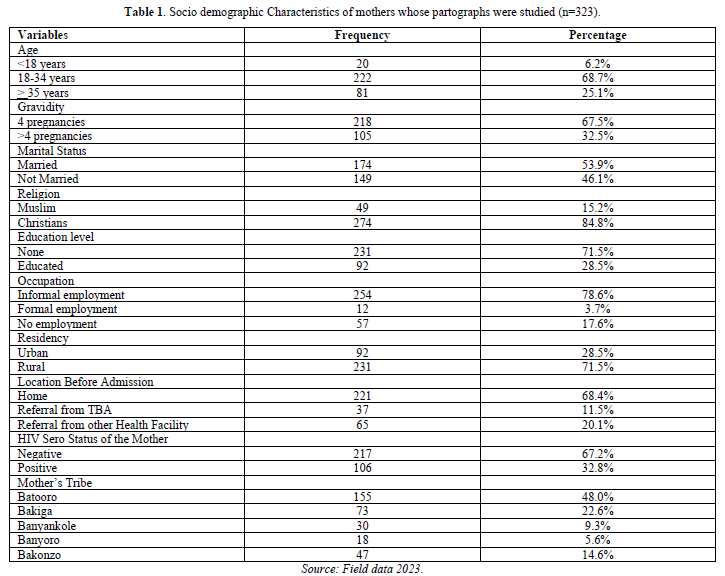
The study examined the socio-demographic characteristics of mothers whose partographs were reviewed. The majority (68.7%) were 18-34 age range, with 53.9% being married and 84.8% identifying as Christians. Gravidity revealed that 67.5% had four or fewer pregnancies, while 71.5% had no formal education. Informal employment was prevalent among 78.6% of participants, and 71.5% resided in rural areas. Before maternity unit admission, 68.4% came directly from home, 11.5% were referred by Traditional Birth Attendants, and 20.1% were referred from other health facilities. Ethnically, the Batooro group comprised the majority (48.0%), and 32.8% were HIV-positive (Table 1).
Mother’s Partograph completeness and correctness
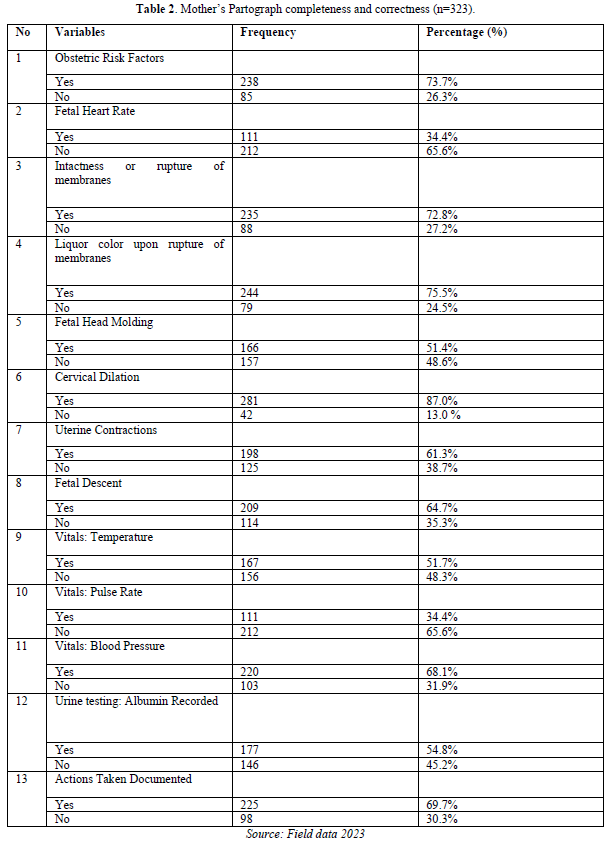
Table 2 presents the completeness and correctness of the partographs used to monitor mothers during labor. The completion rates for various components are as follows: obstetric risk factor assessment had a completion rate of 73.7%, fetal heart rate was at 34.4%, intactness or rupture of membranes had a completion rate of 72.8%, liquor color upon rupture of membranes was completed at 75.5%, fetal head molding had a completion rate of 51.4%, cervical dilation was recorded at 87.0%, uterine contractions had a completion rate of 61.3%, fetal descent completion stood at 64.7%, vitals, such as temperature, were completed in 51.7% of cases, pulse rate was documented at 34.4%, blood pressure was completed in 68.1% of cases, urine testing for albumin was recorded in 54.8% of cases, and actions taken were documented in 69.7% of cases.
Quality of the Partographs
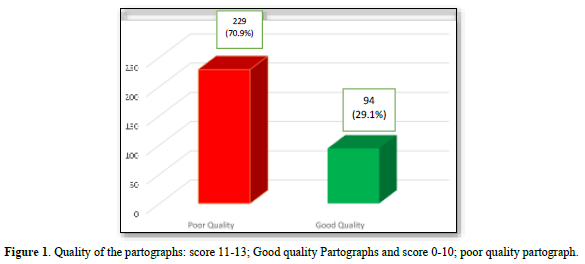
Figure 1 illustrates the quality of the partographs, with the majority being of poor quality at 70.9%, while good quality partographs accounted for 29.1%.
Neonatal Outcomes in relation to Quality of Partograph
Table 3 presents a comprehensive analysis of the correlation between the quality of partographs and various neonatal outcomes. It reveals significant associations between the quality of partographs and several key variables.
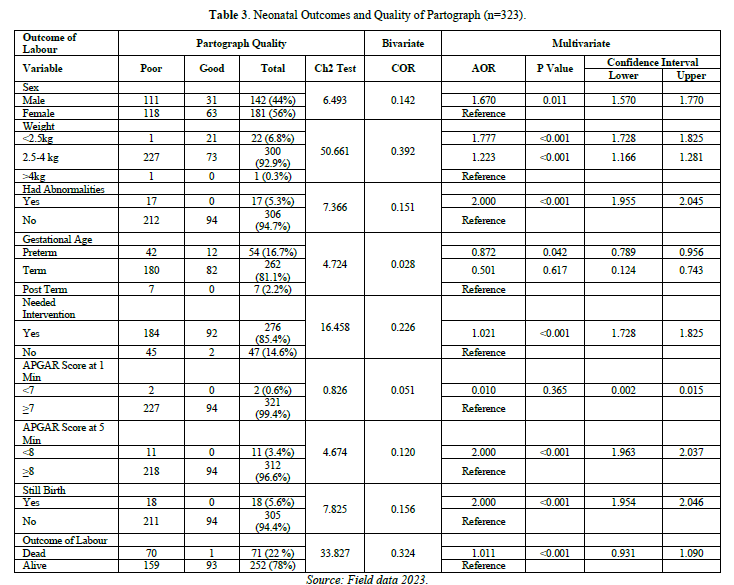
The sex of the neonates was examined, with females representing the majority (56%). Interestingly, male neonates were found to have a 1.670 times higher likelihood of having poor-quality partographs, and this association was statistically significant (p=0.011).
Weight played a vital role, with most neonates (92.9%) falling within the 2.5-4 kg range. Neonates with a weight below 2.5 kg had a significantly increased likelihood (AOR 1.777) of having good-quality partographs, while those in the 2.5-4 kg range had a higher chance (AOR 1.223) of having poor-quality partographs, with a strong statistical significance (p<0.001).
Birth abnormalities were observed in 5.3% of cases, and these neonates consistently had poor-quality partographs. The presence of birth abnormalities was strongly associated with poor-quality partographs, with an AOR of 2.0 and a highly significant p-value (p<0.001).
Gestational age was analyzed, with the majority being term babies (81.1%). Pre-term neonates, constituting 16.7% of cases, had a higher likelihood of having poor-quality partographs (AOR 0.872), which was statistically significant (p=0.042), although the association was moderately weak (Chi-square test = 4.724).
The need for interventions after birth was prevalent among neonates (85.4%) and was significantly associated with poor-quality partographs (AOR 1.021, p<0.001).
The APGAR scores at 1 and 5 min as indicators of neonatal well-being, demonstrated interesting results. The APGAR score at 1 min did not correlate with the quality of partographs. However, at 5 min, APGAR scores below 8 were consistently linked to poor-quality partographs (AOR 2.0, p<0.001).
Stillbirth cases, although relatively rare (5.6%), were uniformly associated with poor-quality partographs (AOR 2.0, p<0.001).
In terms of the general outcome of labor, a clear distinction was observed between neonates born alive (78%) and those who did not survive (22%). The vast majority of neonates who did not survive had poor-quality partographs, leading to a highly significant association (AOR 1.011, p<0.001). Overall, Table 3 provides critical insights into partograph quality and their subsequent impact on neonatal outcomes. These findings underscore the significance of maintaining high-quality partographs throughout labor monitoring for improved perinatal care.
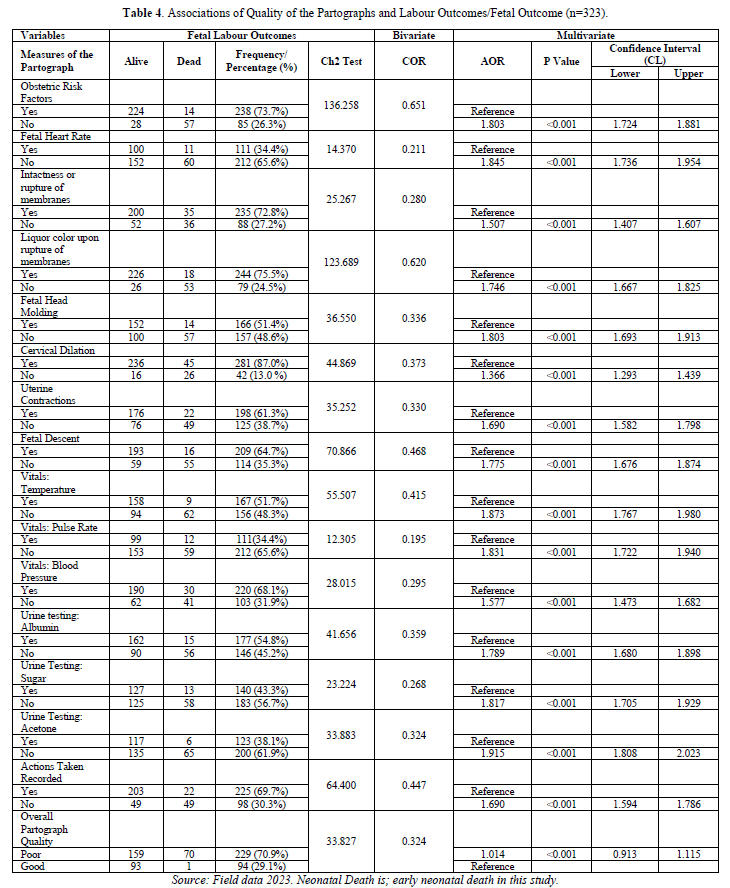
Associations of Quality of the Partographs and Labour Outcomes/Fetal Outcome.
In Table 4 analysis, several aspects of partograph completion were examined in relation to neonatal outcomes. The assessment of obstetric risk factors was well-documented for a majority of mothers (73.7%), and this documentation showed a strong association with positive neonatal outcomes. Neonates whose mothers were not assessed for obstetric risk factors had a significantly higher likelihood of death (AOR 1.803, p<0.001).
Fetal heart rate recording was less frequently documented (34.4%), and its absence had a correlation with neonatal mortality (AOR 1.845, p<0.001). Similarly, the absence of documentation for intactness or rupture of membranes (27.2%) and liquor color upon rupture of membranes (24.5%) was associated with a higher likelihood of neonatal death (AOR 1.746, p<0.001).
Fetal head molding documentation (51.4%) and cervical dilation (87.0%) were well-recorded and had significant associations with neonatal outcomes (AOR 1.803 and AOR 1.366, respectively, both p<0.001). Uterine contractions documentation (61.3%) and fetal descent completion (64.7%) were associated with neonatal mortality (AOR 1.690, p<0.001).
Vital signs documentation, such as temperature (51.7%) and pulse rate (34.4%), had correlations with neonatal death (AOR 1.873 and AOR 1.831, respectively, both p<0.001). Blood pressure documentation (68.1%) was also associated with neonatal outcomes (AOR 1.577, p<0.001).
Urine testing for albumin (54.8%) showed a correlation with neonatal mortality (AOR 1.789, p<0.001). For sugar and acetone urine testing, a lack of documentation had significant correlations with neonatal death (AOR 0.268 and AOR 1.915, respectively, both p<0.001).
The completion of actions taken (69.7%) was significantly associated with neonatal outcomes (AOR 1.690, p<0.001). Overall, the quality of the partograph was predominantly good (70.9%), and poor-quality partographs were correlated with neonatal death (AOR 1.014, p<0.001). In summary, the completeness and correctness of partograph documentation were crucial factors affecting neonatal outcomes, highlighting the importance of thorough and accurate record-keeping in maternal care.
DISCUSSION
Mother’s Partograph completeness and correctness
The completeness and correctness of partographs used to monitor mothers during labor. The findings indicate varying completion rates for different components. Obstetric risk factor assessment was 73.7% complete, fetal heart rate at 34.4%, intactness or rupture of membranes at 72.8%, liquor color upon rupture at 75.5%, fetal head molding at 51.4%, cervical dilation at 87.0%, uterine contractions at 61.3%, fetal descent at 64.7%, vitals like temperature were documented in 51.7%, pulse rate at 34.4%, blood pressure at 68.1%, urine testing for albumin at 54.8%, and actions taken at 69.7% (Table 2).
Level/Magnitude of Partograph Quality.
The majority of the partographs were of poor quality, accounting for 70.9%, while good quality partographs represented 29.1% (Figure 1). The high prevalence of poor-quality partographs can be attributed to various factors related to the mothers, healthcare workers, or the health system. This study's findings align with previous research [7,13,15-20]. However, they contrast with a study conducted in Kamwenge district, where 67.9% of the partographs were of good quality [12]. Possibly due to differences in the scoring criteria used by the authors. Nonetheless, our study finding is consistent with most other studies that have assessed the quality of partographs.
Neonatal Outcomes in relation to Quality of the Partographs
The sex of the neonates was predominantly female, accounting for 56%. There was a correlation of 0.142 between the quality of the partograph and the sex of the neonates. Male neonates had (AOR 1.670, 95% CI:1.570-1.770) for their partographs to be of poor quality, and this association was statistically significant with p=0.011 (Table 3).
This study also observed that the majority of the neonates (92.9%) had a weight between 2.5-4 kgs, followed by those weighing less than 2.5 kgs, which constituted 6.8% of the neonates. A correlation of 0.392 was found between the quality of the partographs and the weight of the neonates. Neonates weighing less than 2.5 kgs had (AOR 1.777, 95% CI: 1.728-1.825) for their partographs to be of good quality, while those weighing between 2.5-4 kgs had (AOR 1.223, 95% CI: 1.166-1.281) for their partographs to be of poor quality. This association was statistically significant with p<0.001 (Table 3). These findings are consistent with a study conducted at Rajashree Chatrapathi Shahu Maharaj Government Medical College, Kolhapur, India, where the majority of neonates had normal birth weight, and a minority had low birth weight [21]. Similar results were also reported in a study at Jawaharlal Nehru Medical College, Ajmer, where most babies were born at term with an average weight of 2.7 kgs [22]. However, these findings contrast with a study conducted in two hospitals in Dar es Salaam city, where newborn birth weight showed no association with the quality of the partographs used for monitoring mothers in labor [23].
All the neonates who had abnormalities, 5.3%, had poor-quality partographs. The presence of birth abnormalities showed a correlation of 0.151 with the quality of the partographs. Neonates with birth abnormalities had (AOR 2.0, 95% CI: 1.955-2.045) for their partographs to be of poor quality, and this association was statistically significant with p<0.001 (Table 3). This finding aligns with a study conducted at Mnazi Mmoja and Vijibweni hospitals in Dar es Salaam, Tanzania [23].
For the gestational age of the neonates, the majority were term babies, accounting for 81.1%, while pre-term births constituted 16.7%. There was a correlation of 0.028 between the quality of the partograph and the gestational age of the neonates. Neonates who were term had (AOR 0.501, 95% CI: 0.124-0.743) for their partographs to be of poor quality, but this association was not statistically significant with a p-value of 0.617. In contrast, neonates who were pre-term had (AOR 0.872, 95% CI: 0.789-0.956) for their partographs to be of poor quality, and this association was statistically significant with a p-value of 0.042 (Table 3). However, it's worth noting that the association was weak, as indicated by the chi-square test result of 4.724. These findings are consistent with a study conducted at Jawaharlal Nehru Medical College, Ajmer [22].
In terms of interventions, the majority of the neonates required interventions after birth, totaling 85.4%. The need for post-birth intervention in neonates correlated at 0.226 with the quality of the partographs. Neonates requiring interventions after birth had (AOR 1.021, 95% CI: 1.728-1.825) for poor-quality partograph completion, and this association was statistically significant with a p-value of less than 0.001 (Table 3). These findings align with a prospective observational study conducted at Rajashree Chatrapathi Shahu Maharaj Government Medical College, Kolhapur, India [21]. However, these findings contrast with the study in two hospitals in Dar es Salaam, where the need for admission to the Neonatal Intensive Care Unit (NICU) showed no association with the quality of the partographs used for monitoring mothers in labor [23]. They also diverge from the study conducted at Jawaharlal Nehru Medical College, Ajmer, where the majority of babies did not require NICU admissions [22]. Additionally, the findings do not align with a study that demonstrated a decrease in neonatal intensive care admissions due to improved monitoring of mothers using partographs [24].
The APGAR score at 1 min revealed that the majority, 99.4%, scored ≥ 7, and no correlation was found between the APGAR score at 1 min and the quality of the partograph. Those neonates with an APGAR score < 7 had (AOR 0.010, 95% CI: 0.002-0.015) for poor-quality partograph completion, and this association was not statistically significant with a p-value of 0.365 (Table 3). These findings do not align with a study conducted in two hospitals in Dar es Salaam, which also showed no association between the quality of the partographs used for monitoring mothers in labor [23].
In the case of the APGAR score at 5 min, the majority, 96.6%, scored ≥ 8, while a minority, 3.4%, had an APGAR score < 8. A correlation of 0.120 was observed between the APGAR score at 5 min and the quality of the partograph. All neonates with an APGAR score < 8 had poor-quality partographs, with an (AOR 2.0, 95% CI: 1.963-2.037) for poor partograph completion, and this association was statistically significant with a p-value of less than 0.001 (Table 3). Again, these findings do not align with the study conducted in two hospitals in Dar es Salaam, which showed no association between partograph quality and the monitoring of mothers in labor [23].
For stillbirth, the majority, 94.4%, did not experience stillbirth, while 5.6% had stillbirth. A correlation of 0.156 was observed between stillbirth and the quality of the partographs. All cases of stillbirth were associated with poor-quality partographs, and experiencing stillbirth had an (AOR 2.0, 95% CI: 1.954-2.046) for poor-quality partograph completion. This association was statistically significant with a p-value of less than 0.001 (Table 3). These findings are consistent with a study conducted in Ethiopia where stillbirth was identified as a major negative outcome [25]. Such outcomes could be attributed to factors such as delays in seeking healthcare due to distance from the hospital or healthcare system-related issues.
In terms of the general outcome of labor, the majority, 78%, resulted in live births, while a minority, 22%, ended in neonatal deaths. A correlation of 0.324 was found between the outcome of labor and the quality of the partographs. Among neonates who did not survive, 99.7% of them were associated with poor-quality partographs. Neonates born alive had an (AOR 1.011, 95% CI: 0.931-1.090) for their partographs to be of poor quality, and this association was statistically significant with a p-value of less than 0.001 (Table 3). These results contrast with a study conducted in Matuail, Dhaka, Bangladesh, which emphasized the importance of quality monitoring of mothers during labor and reported reduced neonatal complications and mortality. In their study, they observed significantly lower neonatal deaths [26].
Associations of Quality of the Partographs and Labour Outcomes/Fetal Outcome.
Obstetric Risk Factors Assessment: The majority of mothers, 73.7%, had obstetric risk factors assessed, while 26.3% were not assessed. There was a strong correlation, 0.651, between the documentation of obstetric risk factor assessment and the fetal labor outcome, and this association was highly significant with a chi-square test result of 136.258. Neonates who were not assessed for obstetric risk factors had an (AOR 1.803, 95% CI: 1.724-1.881) for neonatal mortality, which was statistically significant with p<0.001 (Table 4). This finding underscores the importance of assessing obstetric risk factors during labor monitoring to prevent complications that can lead to both fetal and maternal death. However, it does not align with previous studies [12,23].
Fetal Heart Rate: The majority of mothers, 65.6%, did not have fetal heart rate recorded, while 34.4% had it recorded. A correlation of 0.211 was observed between fetal heart rate recording and neonatal outcomes (alive or dead). Neonates whose mother's charts lacked fetal heart rate recording had an (AOR 1.845, 95% CI: 1.736-1.954) for neonatal mortality, and this was statistically significant with p<0.001 (Table 4). Proper monitoring of fetal heart rate during labor is essential to detect distress, which can lead to neonatal mortality. This finding contrasts with a study conducted in a hospital in Katsina, Nigeria, where most charts had recordings and was associated with positive neonatal outcomes [20].
Intactness or Rupture of Membranes: Among mothers, 72.8% had documentation of intactness or rupture of membranes, while 27.2% did not. A correlation of 0.280 was observed between the documentation of intactness or rupture of membranes and labor outcomes. Neonates whose mother's charts lacked documentation for intactness or rupture of membranes had an (AOR 1.746, 95% CI: 1.407-1.607) for neonatal mortality, and this was statistically significant with p<0.001 (Table 4). The lack of documentation may result in infection or oligohydramnios, which necessitates monitoring through ultrasound scans and possibly a caesarean section. These findings contrast with previous studies [23,27,28].
Liquor Color Upon Rupture of Membranes: Liquor color upon rupture of membranes was documented in the majority, 75.5%, and not documented in 24.5% of cases. A strong correlation of 0.620 was observed between the lack of documentation of liquor color upon rupture of membranes and neonatal outcomes. Neonates whose mother's charts lacked documentation for liquor color upon rupture of membranes had an (AOR 1.746, 95% CI: 1.667-1.825) for neonatal mortality, and this was statistically significant with p<0.001 (Table 4). The absence of documentation might indicate meconium-stained liquor, possibly indicating fetal distress, leading to neonatal mortality. These findings do not align with previous studies [23,27,28].
Fetal Head Molding: Records of fetal head molding was found in 51.4% of cases and absent in 48.6%. A correlation of 0.373 was observed between the lack of documentation of fetal head molding and neonatal outcomes. Neonates whose mother's charts lacked documentation for fetal head molding had an (AOR 1.803, 95% CI: 1.693-1.913) for neonatal mortality, and this was statistically significant with p<0.001 (Table 4). Failure to document fetal head station could lead to prolonged labor and fetal distress. These findings do not align with previous studies [23,27,28].
Cervical Dilation: Among the mothers, 87.0% had records of cervical dilation, while 13.0% did not. A correlation of 0.373 was observed between the lack of documentation of cervical dilation and neonatal outcomes. Neonates whose mother's charts lacked documentation for cervical dilation had an (AOR 1.366, 95% CI: 1.293-1.439) for neonatal mortality, and this was statistically significant with p<0.001 (Table 4). Failure to monitor cervical dilation may result in poor progress of labor, leading to fetal distress and neonatal death. These findings do not align with previous studies [23,27,28].
Uterine Contractions: Records of uterine contractions were found in 61.3% of cases, while 38.7% had no records. A correlation of 0.330 was observed between the lack of documentation of uterine contractions and neonatal outcomes. Neonates whose mother's charts lacked documentation had an (AOR 1.690, 95% CI: 1.582-1.798) for neonatal mortality, and this was statistically significant with p<0.001 (Table 4). In cases where uterine contractions were not documented, midwives were unable to assess the strength and progress of labor, which might have resulted in fetal distress. These findings do not align with previous studies [23,27,28].
Fetal Descent: Records of fetal descent were found in 64.7% of cases, while 35.3% had no records. A correlation of 0.468 was observed between the lack of documentation of fetal descent and neonatal outcomes. Neonates whose mother's charts lacked documentation for fetal descent had an (AOR 1.690, 95% CI: 1.676-1.874) for neonatal mortality, and this was statistically significant with p<0.001 (Table 4). Failure to document fetal descent might result in fetal aspiration or prolonged labor, leading to fetal distress and neonatal mortality. These findings do not align with previous studies [23,27,28].
Vitals: Temperature: Of all the charts, 51.7% had recorded temperature, while 48.3% did not. There was a correlation of 0.415 between the recording of temperature charts and the outcome of labor, whether the neonate was alive or deceased. Neonates whose mothers' vital signs, specifically temperature, were not recorded had an (AOR 1.873, 95% CI:1.767-1.980) for neonatal mortality, and this was statistically significant with p<0.001 (Table 4). The absence of temperature recording may indicate maternal infection or sepsis, possibly leading to neonatal infection and distress, ultimately resulting in neonatal death. These findings do not align with previous studies [23,27,28].
Vitals: Pulse Rate: The majority, 65.6%, had not recorded vital signs for pulse rate, while a few, 34.4%, had this recorded. A correlation of 0.195 was observed between the lack of pulse rate recording and the outcome of labor (whether the neonate was alive or deceased). Neonates whose mothers' charts did not contain pulse rate recordings had an (AOR 1.831, 95% CI: 1.722-1.940) for neonatal mortality, which was statistically significant with p<0.001. Additionally, for vital signs: blood pressure, 68.1% had this recorded in the mother's charts, while 31.9% did not. There was a correlation between blood pressure documentation and the outcome of labor (whether the neonate was alive or deceased). Neonates whose mothers' charts were not recorded for blood pressure had an (AOR 1.577, 95% CI: 1.473-1.682) for neonatal mortality, which was statistically significant with p<0.001 (Table 4). In cases where pulse rate and blood pressure were not documented, it could be inferred that the mothers may have had pre-eclampsia, which affected the fetus and led to mortality. These findings, however, do not align with previous studies [23,27,28].
Urine Testing for Albumin: Among the records, 54.8% contained documentation of urine testing for albumin, while 45.2% did not. There was a correlation of 0.359 between the presence of urine testing records for albumin and the outcome of labor (whether the neonate was alive or deceased). Neonates whose mother's charts lacked documentation for urine testing of albumin had an (AOR 1.789, 95% CI: 1.680-1.898) for neonatal mortality, but this was not statistically significant with p<0.001 (Table 4). It is possible that neonates who died may have been affected by their mothers' proteinuria due to pre-eclampsia during labor. These findings do not align with previous studies [23,27,28].
Urine Testing: Sugar: Of the records, 56.7% did not contain documentation of urine testing for sugar, while 43.3% had this documented. There was a correlation of 0.268 between the absence of urine testing records for sugar and the outcome of labor (whether the neonate was alive or deceased). Neonates whose mothers' charts lacked documentation for urine testing of sugar had an (AOR 1.817, 95% CI:1.705-1.929) for neonatal mortality, and this was statistically significant with p<0.001 (Table 4). It is possible that the mothers of the deceased neonates had diabetes mellitus, which affected the fetuses along with other factors like fetal distress. These findings do not align with the study by Sospeter [23], Vogel [27] and Mwaka [28].
Urine Testing: Acetone: A majority, 61.9%, had no records of urine testing for acetone, while 38.1% had these records documented. There was a correlation of 0.324 between the absence of urine testing records for acetone and the outcome of labor (whether the neonate was alive or deceased). Neonates whose mothers' charts lacked documentation for urine testing of acetone had an (AOR 1.915, 95% CI: 1.808-2.023) for neonatal mortality, and this was statistically significant with p<0.001 (Table 4). These findings do not align with the studies by Sospeter [23], Vogel [27] and Mwaka [28].
Actions Taken: Records of actions taken were present in 69.7% of cases and absent in 30.3%. There was a correlation of 0.447 between the absence of recorded actions taken and the outcome of labor (whether the neonate was alive or deceased). Neonates whose mother's charts lacked documentation of actions taken had an (AOR 1.690, 95% CI: 1.594-1.786) for neonatal mortality, and this was statistically significant with p<0.001 (Table 4). It is possible that in cases where no actions were recorded, the neonates may not have been properly monitored, or midwives may have been overwhelmed with the number of mothers to attend to. These findings do not align with the study by Sospeter [23], Vogel [27] and Mwaka [28].
For the overall partograph quality: 70.9% were of poor quality, and 29.1% were of good quality. There was a correlation of 0.324 between the overall quality of the partograph and the outcome of labor (alive or dead). Neonates whose mothers' charts were of poor quality had an (AOR 1.014, 95% CI: 0.913-1.115) for death, and it was statistically significant with p<0.001 (Table 4). This aligns with the study conducted in the hospitals of Mohali and Patiala districts of Punjab, India [29], as well as the study conducted in a hospital in Katsina, Nigeria, where good quality partographs were associated with positive neonatal outcomes of labor [20]. These findings are also consistent with a study in Zambia [28]. However, they do not align with the study conducted in six health facilities in Kamwenge district, which found no association between the quality of the partographs and neonatal outcomes [12]. These results are in line with a prospective observational study conducted at a tertiary care teaching institute, KMCT Medical College in Kozhikode [30].
CONCLUSIONS
The quality of partographs in the hospital was exceptionally low, with the majority of them being of poor quality.
The principal fetal outcomes of labor among newborns whose mothers' partographs were assessed included low neonatal birth weight, neonatal abnormalities at birth, pre-term neonatal gestational age, neonatal need for intervention after birth, APGAR scores < 8 at 5 min, stillbirth, and early neonatal death.
This study has revealed significant associations between partograph quality and neonatal outcomes. There was a significant correlation between poor-quality partographs and neonates who did not survive (early neonatal death plus stillbirth).
RECOMMENDATIONS
Based on the study findings, the following recommendations are proposed:
Healthcare providers should receive additional training and support in maintaining accurate and complete partograph records, with particular attention to male neonates, pre-term neonates, and those with birth abnormalities.
Regular audits and quality improvement initiatives should be implemented to monitor partograph completion and ensure that it adheres to best practices.
Healthcare facilities should provide guidelines and resources to assist in the consistent and comprehensive documentation of partographs, especially in cases involving interventions and neonatal complications.
Emphasis should be placed on the importance of documenting all relevant parameters during labor, especially those with strong associations with neonatal outcomes, such as the APGAR score at 5 min.
Overall, these recommendations aim to enhance the quality of partograph completion and, subsequently, improve neonatal outcomes, particularly for vulnerable neonates and those facing complications during birth.
FURTHER DIRECTION
The study recommends a study to explore the specific factors contributing to the disparities in partograph quality and neonatal outcomes, enabling the development of targeted interventions.
ACKNOWLEDGEMENT
We acknowledge the dedication and resilience of healthcare workers in the maternity Unit at Fort Portal Regional Referral Hospital. Additionally, we acknowledge Komase EbeNezer REsearch CenTre Limited (KoNET) for Implementing and cultivating the environment that enabled this partograph study to be conducted that resulted to the development of this manuscript. We also extend our heartfelt thanks to well-wishers and friends for their support.
CONTRIBUTORS
David Francis Olebo, affiliations; KOMASE Ebenezer Research Centre Limited (KoNET) and Makerere University Walter Reed Project, Uganda. conceive, designed, implemented the project, analyzed the data and drafted the manuscript.
Enos Mirembe Masereka, affiliations; Mountains of the Moon University Supervised the Project, reviewed and edited the manuscript.
Brenda Night Muhindo, affiliations; Makerere University Walter Reed Project. Conceive, implemented the project, supervised data collection, reviewed and edited the manuscript.
Mubaraka Kayiira, affiliations; Infectious Disease Institute (IDI), Uganda reviewed and edited the manuscript.
Jacqueline Nalikka, affiliations; Makerere University Walter Reed Project, reviewed and edited the manuscript.
The final manuscript has been reviewed and approved by all the authors.
FUNDING
This work was funded by the authors themselves and no external individual or organization funded it. However, the partograph Study Project was implemented under Komase EbeNezer REsearch CenTre Limited (KoNET).
COMPETING INTERESTS
The authors do not have any conflict of interest in this research.
ETHICS APPROVAL
The research work was approved by Mountains of the Moon University Ethics committee and informed consent to review; the partographs was obtained.
DATA AVAILABILITY STATEMENT
All the relevant data in this study have been analyzed and reported in the article but data set can be availed on request.
SUPPLEMENTAL MATERIAL
Not Applicable.
No Files Found
Share Your Publication :