-
Publish Your Research/Review Articles in our High Quality Journal for just USD $99*+Taxes( *T&C Apply)
Offer Ends On
Sergio Dus* and Filippo Dus
Corresponding Author: Sergio Dus, Dusmedical clinic, 4 33077 Sacile PN, Italy.
Received: August 01, 2023 ; Revised: August 19, 2023 ; Accepted: August 22, 2023 ; Available Online: September 26, 2023
Citation: Dus S & Dus F. (2023) The Role of Surgery in TMD. J Oral Health Dent Res, 3(3): 1-8.
Copyrights: ©2023 Dus S & Dus F. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Views & Citations
Likes & Shares
Nowadays the Temporomandibular disorder are present in almost 20% of people in industrialized countries and women are more affected than men. TMD are strongly related to hectic life and excessive stress. Internal derangement (I D) is a frequent problem found in TMD.
Internal Derangement is a general orthopedic term implying a mechanical fault that interferes with the smooth action of a joint. The incoordination condilo discale or Internal Derangement (ID) is one of the most frequent pathology involving ATM. Included in this pathology there are click, lock, osteoarthrosis and jaw dislocation. This term (ID) means the complete loss of physiological articular relation between disc, condyle and glenoid fossa of temporal bone during the physiological movement of the jaw. The etiology looks to be represented by factors like mechanical stress leading to non-adaptive answers resulting in the pathogenesis of TMD. Mechanical stresses that exceed the tolerance of the joint tissue lead to direct mechanical injury to the tissues with inflammation and hypoxia-riperfusion. When conservative therapy fails to resolve the symptoms and there is a fatal functional alteration, should be used at various intraarticular surgical therapies that have shown after many years of follow-up, satisfactory results even if the literature sometimes presents conflicting opinions. The primary role of surgery is to reduce the symptoms, pain and improve joint function. The purpose of this study is to compare our experience and our clinical data of 25 years of open surgical technique of ID made in the inferior compartment rebuilding the lateral ligament of the disk with the suture of any disc perforation or retrodiscal tissue, preceded by an arthroscopy with washing in upper compartment also treating most patients bilaterally; with recent literature by checking the various surgical techniques used to correct the ID and the follow-up of the last years to clarify whether and what are the effective surgery to eliminate or drastically reduce the symptoms of this disease of the temporo-mandibular joint after the failure or combined with conservative therapies and which is the preferred technique ranging from the less invasive (arthroplasty and arthrocentesis) to open, dependents on diagnosis.
INTRODUCTION
Correlation Between Occlusion and Posture in TMD
Today more than ever, in order to properly understand and evaluate the loads and forces transmitted during chewing, but above all from the parafunctional to the various detoalveolar, implant, articular and musculoskeletal structures, it is necessary to know well how the stomatognathic system works and the role that it plays in the posture of the patient. For this reason, an accurate evaluation of the patient must be made to exclude hypothetical dysfunctional patients.
The patient with temporomandibular disorders (TMD) should first treat the pathology and then start a prosthetic implant treatment plan. At the beginning of the eighties, when I was just twenty, I began to be interested in the biomechanics of the stomatognathic system, which is made up of a set of structures involved in mandibular movements and in chewing, but above all in discharging tension and stress through the parafunctions, characteristic of busy life of people. The main elements of this system are the temporomandibular joint (TMJ), the basal bones (maxilla and mandible), the dento alveolar system, the first cervical vertebrae and the neuromuscular system.
Already in those years, the problems that inevitably arose in many patients were beginning to be understood, linked to tensions and stress, which weighed heavily on the stomatognathic system causing some pathologies, such as ear pain, headaches, cervical and solders pain and limitation of mandibular movement. The cause of articular and musculoskeletal pathologies of the whole body began to be attributed to the occlusion, working more often in the search for the ideal occlusion in order to be able to avoid and even resolve these pathologies, even distant from the buccal area. An attempt was made to obtain perfect occlusion by searching for centric tripod or bipod stops, with the aid of pantographic and subsequently axiographic recordings, which had the purpose of detecting joint, protrusive and laterotrusive movements (mediotrusion and laterotrusion) to adjust the inclination of the joint eminence and Bennett's angle in the individual articulator as well as with the fitting of the models aided by the kinematic face bow, which could mirror 97% of the patient's individual movements. However, the methods of research and treatment of TMD patients were not fully understood. Stress and daily parafunctions overload the oro-maxillofacial system, which is one of the first districts to be affected by the problems associated with these factors. There are an estimated 65,000 daily stressors and the mouth is the alarm bell for other pathological conditions with more than 750 million people suffering from anxiety and depression in developed countries.
TMDs are a diverse group of musculoskeletal and neuromuscular conditions involving the TMJ complex, surrounding musculature, and bone components. TMDs affect up to 15% of adults, with a peak incidence between 20 and 40 years of age and are much more common in women. The main symptoms include jaw pain and dysfunction, earache, headache with craniofacial pain involving the masticatory muscles and the muscular innervations of the head and neck, and can range from a slight annoyance with noise (clicking), to debilitating pain, dizziness, limitations or blockages of joint function which over the years can lead to osteoarthritis of the TMJ.
The etiology of TMDs is multifactorial and includes a biological, environmental, social, emotional, and cognitive origin. Diagnosis is often based on history and physical examination. Diagnostic imaging can be useful when malocclusion, intra-articular anomalies, malformations, or tumors are suspected. TMDs are a major cause of non-dental pain in the orofacial region and carry a significant economic burden of absence from work. Most patients improve with a combination of noninvasive therapies, including patient education, self-care, cognitive behavioral therapy (s-EMG biofeedback), drug therapy, physical therapy, and occlusion devices. Only in a small percentage (1-2%) of cases, it is necessary to resort to more invasive treatments ranging from arthrocentesis (washing) to open joint surgery. Nonsteroidal anti-inflammatory and muscle relaxants are recommended initially, while benzodiazepines or antidepressants may be added for chronic cases. Being a multifactorial pathology, it must be treated with a multidisciplinary approach that requires collaboration between a surgeon, dentist, a physiotherapist and, in some cases, a psychotherapist.
MATERIALS AND METHODS
This work was performed using the MEDLINE bibliographic database, with a combination of keywords, such as "TMJ surgery", "internal derangement", "temporomandibular joint dysfunction", "temporomandibular disorder". Works of surgical interest were collected and selected favoring only those in English. The search was restricted to the last few years and the keywords were limited to the text and the title of the article. Subsequently, the selected articles were compared with the data in our possession, to have a real comparison between the international literature and the follow-up of our clinical cases. Furthermore, articles published by us were included in the bibliographic search, also considering our personal clinical experience in collaboration with Prof. Piero Cascone and the staff of the Department of Odontostomatological and Maxillofacial Sciences of the University of Rome "La Sapienza".
Etiopathogenesis of TMDs
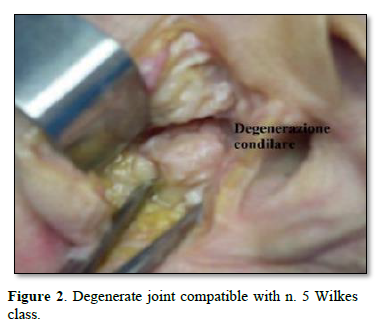
80% of TMDs are more common in females. These disorders appear to be due to mechanical stresses which, with maladaptive responses, lead to the pathogenesis of TMD. Mechanical stresses that exceed joint tissue tolerance lead to direct mechanical tissue damage, with inflammation and hypoxia-reperfusion. The resulting synovitis leads to release of Interleukin-1, formation of collagen I and III and fibronectin, resulting in fibrosis of the synovial membrane (Figures 1 & 2). As far as dislocation is concerned, it is linked to muscular dyssynergia due to an altered synchrony and synergy of the masticatory muscles (agonists and antagonists) and to an articular ligament laxity which determines a considerable freedom of movement of the condyle [1-3].

CLASSIFICATION OF INTERNAL DERANGEMENT - WILKES CLASSIFICATION
It is based on 3 evidences: clinical (C), radiological (R) and surgical (S) [4,5].
C: No symptoms, slight click, no pain, no functional limitation
R: Slight displacement, normal tomograms
S: Slight anterior displacement, normal anatomy
C: Appearance of temporal pain and mechanical problems, increased noise
R: Slight anterior displacement, early anatomical disc deformity, normal tomograms
S: Dislocation, early anatomical deformity (slight posterior margin thickening), well-defined central joint area
C: Frequent and variable pain, temporal migraine, mechanical symptoms (closed lock), difficulty in functional movements with pain
R: Dislocation with significant anatomical deformity or disc prolapse, normal tomograms
S: Marked anatomical deformity with dislocation, variable adhesions without hard tissue alteration
C: Chronicity of variable and episodic pain, cranio-mandibular pain, variable limitation of movement, alternating course
R: Abnormal tomograms, initial to moderate degenerative remodeling with hard tissue change
S: Degenerative changes and hard tissue remodeling, osteophytic projections, multiple adhesions, no retro disc tissue perforation
C: Crepitus on examination (classic sign of osteoarthritis), rubbing, variable and episodic pain, chronic limitation of movement with functional difficulty
R: Displacement, perforation with simultaneous filling of the upper and lower compartments, gross disc and hard tissue deformities, abnormal tomograms with essential arthritic degenerative changes
S: Gross degenerative changes of the disc and hard tissue, with perforation of the posterior attachment, erosions of surfaces with multiple adhesions equivalent to degenerative arthritis (sclerosis, flattening and change of the condylar shape to anvil, osteophytic projections and subchondral cyst formations)
Surgical techniques:
The surgical techniques used in the ID have undergone a considerable evolution over the years which includes:
Humprey 1856: Notes on condylotomy
Annandale 1887: Notes on the reduction and anchoring of the articular disc
Lanz 1909: Notes on meniscectomy
Silver 195: Adoption of meniscectomy which was widely used for 40 years with good results
Farrer and McCarty 1970: Introduction of the concept of ID
Ohnishi 1975: TMJ artoscopy
Chino, Nitzan and Cascone 1985-1988: Surgical purpose and restoration of the physiological morphofunctional relationship of the ATM;
Nitzan et al. 1991: Arthrocentesis
McCain et al. 1992: Malocclusion as a common occurrence of ID with arthroscopic repositioning and suturing of the disc
Cascone 1985: Open functional surgery of ATM
Condilar Shaving (arthroscopy diagnostic arthrocentesis, high condylotomy, disc repositioning with suture).
The primary role of surgery is the physical cleansing, repair, and removal of diseased tissue that causes pain and TMJ dysfunction. Consequently, the primary objective of surgery is to reduce pain symptoms and improve joint function. More the symptoms are localized to the TMJ region, more effective is the surgery. Based on Schwartz's psychophysiological theory of joint pain, Laskin introduced the term myofascial pain and dysfunction to distinguish between TMD patients with predominantly muscle symptoms and those with joint-type symptoms. This simple concept significantly improves diagnostic awareness of the distinction between the two groups of TMD patients. Patients with myofascial pain, of course, are not candidates for surgery, while those with joint symptoms (I D. the most common) can generally be considered potential surgical candidates.
In clinical practice, most patients present with a combination of muscle and joint problems; in this case a careful evaluation is required to determine which of the two is the primary or dominant component and which is the secondary or reactive component. Therefore, if the muscle component is the primary cause, the patient should be approached with a conservative method before the opportunity to perform surgery can be appropriately evaluated. Conversely, when muscle symptoms derive primarily to a joint problem, attention should be focused on the joint which properly treated should lead to spontaneous resolution of muscle symptoms.
INDICATIONS FOR TMJ SURGERY
Indications for surgical therapy in the management of TMDs can be classified into relative and absolute. Absolute indications are reserved for cases in which surgery plays an undisputed central role, includes rare disorders such as tumors, growth abnormalities and TMJ ankyloses [6-10].
Relative indications are for cases where surgery has a less clearly defined role, particularly where non-surgical management plays a predominant role. Indications regarding surgery in the management of TMJ disorders are important as they address the most common disorders, namely joint ID involving integrity, disc position and osteoarthritis. In the literature, the first indication for TMJ surgery is failure of non-surgical therapy.
Unfortunately, failure of conventional non-surgical therapy can often be the result of misdiagnosis or incomplete diagnosis which occurs in 20% of patients treated with conservative therapy in TMDs. This value far exceeds the 5%, which represents the percentage often cited in the literature, of TMD patients undergoing surgery. What the literature often fails to point out is that approximately 75% of patients who fail to respond to nonsurgical treatment are also not suitable candidates for surgery. Furthermore, the failure of non-surgical treatment as a precondition for surgery is questionable since non-invasive treatment modalities, such as arthrocentesis and TMJ arthroscopy, may be considered as the first treatment option in the first months in cases such as the closed lock. What distinguishes candidates for surgery from the rest of the group in which nonsurgical treatment failure has occurred are the clinical presentation and radiological features of the disease. The main clinical features of potential candidates for surgery include pain symptoms and localized TMJ dysfunction. The dysfunction may include painful joint clicking, crepitus (osteoarthritis), or joint weakness (closed lock). In the absence of pain, the severity of the dysfunction should be considered in terms of the patient's reported degree of disability. Surgery should ideally be evaluated on the basis of objective criteria, for example a patient's maximum inter-incisal opening sufficient for routine dental care. Historical evidence suggests that TMJ dysfunction is not always a progressive disease, so short-term relief may be achieved with medication or arthrocentesis depending on the diagnosis.
Radiological findings should never be interpreted in isolation. The decision for surgery should be based primarily on the clinical findings in relation to factors such as the impact of the disease on the patient's well-being and the prognosis of the disease if it is not treated surgically. Radiological investigations should only play a supporting role. The literature would seem to support that surgery for common TMDs, such as internal TMJ changes and osteoarthritis, is being considered in two main conditions. The first is when the TMD is refractory to appropriate nonsurgical therapy; the second exists when the TMJ is the source of the pain and/or dysfunction that involves significant damage to the patient.
According to the literature, TMJ issues such as closed lock is effectively managed with arthrocentesis (in the case of acute closed lock) and arthroscopy (in the case of chronic closed lock). Painful TMJ issues in which there is little restriction of mandibular function (reducing disc displacement) would appear to respond to condylotomy procedures, where condylar reduction results in an increase in joint space with relief of intra-articular pressure. TMJ arthrotomy is reserved for the advanced stages of intra-articular and osteoarthritic problems.
The overall quality of the TMJ surgery literature is sub-optimal. Randomized clinical trials comparing surgical treatment of TMDs with medical treatment and no treatment (the placebo effect) do not exist. Because such studies are impractical, the true benefit of surgical treatment of TMDs can never be definitively established. Reston and Turkelson conducted a meta-analysis suggesting that TMJ arthrocentesis and arthroscopy are effective in the management of patients with disc displacement without reduction. Even if the studies up to now present in the literature are not optimal, the results cannot be ignored. Therefore, current recommendations for surgery must be based on the best available evidence while waiting for better designed, controlled, randomized placebo clinical trials to guide the best decision for both physicians and patients.
OPEN FUNCTIONAL SURGERY OF THE TMJ ACCORDING TO CASCONE TECHNIQUE
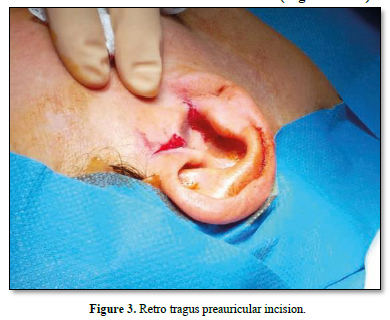
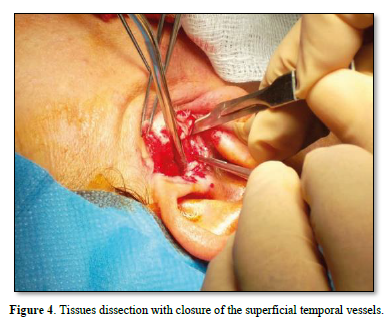
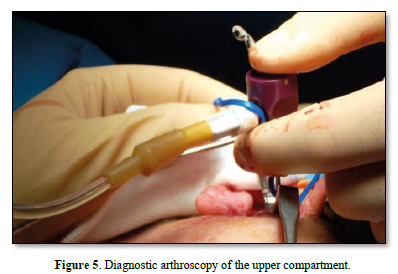
TMJ forms anatomical relationships with adjacent structures such as the facial nerve infero-laterally, the auriculo-temporal nerve and the superficial temporal vessels posteriorly and infero-medially with the internal maxillary artery. This type of surgery involves an arthroplasty with high condilectomy and the repositioning of the articular disc precede by a diagnostic arthroscopy. After the preauricoular incision retrotragus, subsequently the deep fascia of the temporal muscle is exposed and the joint capsule is visualized. Closure of the superficial temporal vessels is completed with preservation of the auriculotemporal nerve. Now the diagnostic arthroscopy of the upper compartment is performed as usual, which can help us resolve both diagnostic doubts in the event of a difficult pathology and doubts that may emerge from the instrumental tests performed. This arthroscopic approach is preceded by the insertion of the needle of a syringe containing lactate ringer, which serves not only to find the upper joint compartment by exploiting the pumping effect, but also to distend and increase the joint space by detaching any fibrillar adhesions. Once this procedure has been performed, the trocar cannula of the one-point arthroscope is inserted near the needle and we will be able to notice the leakage of the liquid previously injected with the syringe; this sign ensures that you are within the superior articular compartment. The trocar, in addition to having the channel for inserting the optics, has a service channel for irrigation which thus allows a sort of preoperative arthrocentesis to be performed, where the needle initially used with the lactate ringer will be used for the outflow of the abundant washing performed during the arthrocentesis, until the clear liquid will come out, a clear sign of cleanliness of the joint compartment, in this way it will be easier to perform the arthroscopy by visualizing the anatomical structures such as the upper surface of the disc, the retrodiscal bilaminar area, the glenoid cavity and articular tubercle. The visible alterations may include erosions of the articular fibrocartilage that can reach the exposure of the bone surface, the degree of dislocation of the disc and any perforations of the retro-disc tissue and less frequently of the disc; the difference between the two is that in the first we see irregular margins with microvascular structures, while in the disc the margins are clear-cut, thick and whitish in color. Perforations are always accompanied by synovial outpourings which can make difficult endoscopic vision. In the presence of perforations, the vision of the lower compartment also becomes possible where it is often possible to notice erosions or solutions of continuity of the fibrocartilage that covers the head of the condyle.
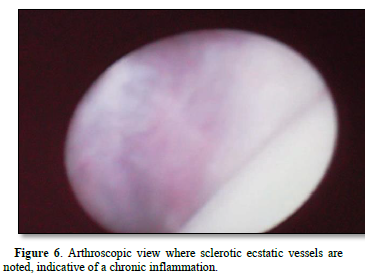
Evaluating the degree of dislocation of the disc in the internal derangement, the space normally intended for the disc is almost completely occupied by the retro-disc tissue or the totally remodeled posterior bilaminar area, which appears full of small vessels and milky white in color. It is also necessary to check the state of the synovium, which is often inflamed and edematous with an increase in ecstatic blood vessels, tortuous and easily bleed, while in long-standing alterations, hairy outpourings are frequently found on its surface.
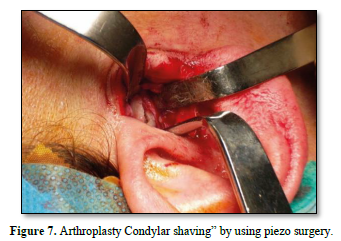
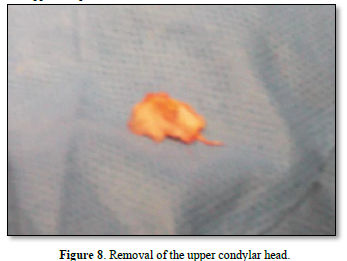
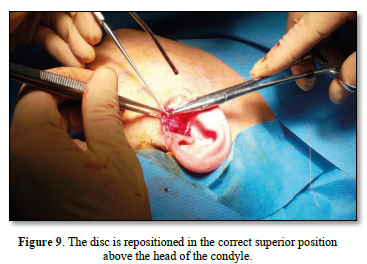
Once the diagnostic arthroscopy is complete, arthroplasty is performed with a "condylar shaving" using piezo surgery to avoid leaving residues of metal powder inside the joint, which could create artifacts in the MRI. The disc is then repositioned from the pathological anteromedial position to a correct superior position above the head of the condyle. The fixation of the disc to the head of the condyle is performed by making a hole on the lateral tubercol of the condyle fixed using the MITEK® Microfix Quick Anchor Plus1.3 package with the microanchor inside. The anchor is connected to a non-absorbable 3.0 Ethibond suture, which is used to fix the posterolateral side of the disc in physiological position.
A functional test of the joint's mobility is then performed by opening and closing the jaw and moving it from side to side, checking that the disc preserves the repositioning performed. Subcutaneous and preauricular skin sutures are then performed. In the post-operative course, soft or semi-liquid feeding is foreseen for the first 7 days; subsequently, a functional stimulation of the ATM is implemented through active and passive physiotherapy exercises (Figures 3-10).

RESULTS
Our data:
565 patients treated from 1982 to 2005 at the MF Surgery of the University of Rome "La Sapienza".
352 patients (62.3%) contacted for follow-up visits: 299 females (85%) and 53 males (15%)
337 patients bilateral ID, 22 unilateral ID
696 joints treated
Age between 16-68 with an average value of 32 years
Follow-up from 3 to 26 years with a mean value of 12.5 years
Local pain (TMJ):
Headache and neck/shoulder pain:
All Patient increased maximum opening of the mouth.
CONCLUSIONS
From the above, comparing our experience and clinical data with the international literature, we can conclude that:
No Files Found
Share Your Publication :